Coronavirus Vaccine & Herd Immunity Digest #2 by Bruce Brown
News & Commentary for People Planning to Survive the Coronavirus Pandemic
New and interesting Updated August 14, 2020
- Sweden’s top virologist has a message on how to defeat coronavirus: Open schools and no masks, Fortune
- Children and the virus: As schools reopen, much remains unknown about the risk to kids and the peril they pose to others, Washington Post
- Russia gears up for mass vaccination against coronavirus despite international skepticism, CNBC
- Dozens of COVID-19 vaccines are in development. Here are the ones to follow, National Geographic
- Study says actual number of Covid-19 cases is far greater than thought, CNN
- Revealed: Seven year coronavirus trail from mine deaths to a Wuhan lab, Times of London (England)
- Nobel Laureate Calls COVID-19 Manmade, CNews (France)
- The people with hidden immunity against Covid-19, BBC (England)
- Pets show antibodies to SARS-CoV-2 in Italian study, Medical Life Sciences News
Past Digests
- Coronavirus Vaccine & Herd Immunity Digest #1 (March – July 2020)
- Coronavirus Vaccine & Herd Immunity Digest #2 (July – August 2020)
- Coronavirus Vaccine & Herd Immunity Digest #3 (August – September 2020)
Top commentary
- Do Not Fear the (coronavirus) Wolf, by Bruce Brown
- Bruce Brown reviews COVID-19 news coverage in media such as the New York Times, Washington Post, CNN, Fortune, National Geographic, etc.
Historical context
- A Journal of the Plague Year, by Daniel Defoe: Then (1665) & Now (2020)
Index of Articles in chronological order
- World’s first recorded case of a child contracting COVID-19 from its mother inside the womb, Business Insider, 7/14/2020
- A Look at the Reinfection Rate, National Review, 7/14/2020
- Florida tops its single-day record for coronavirus deaths, but death rate falls through floor to less than 1%, 7/14/2020
- An mRNA Vaccine against SARS-CoV-2 — Preliminary Report, New England Journal of Medicine, 7/14/2020
- How a False Hydroxychloroquine Narrative Was Created, Mercola.com, 7/15/2020 (Commentary)
- Your Ancestors Knew Death in Ways You Never Will, New York Times, 7/15/2020 (Commentary)
- The coronavirus pandemic most resembles the 1957 Asian flu pandemic, Coronavirus Vaccine & Herd Immunity Digest, 7/16/2020
- Nobel Laureate Calls COVID-19 Manmade, CNews, 7/17/2020 (Commentary)
- State Department releases cable that launched claims that coronavirus escaped from Chinese lab, Washington Post, 7/18/2020 (Commentary)
- The people with hidden immunity against Covid-19, BBC, 7/19/2020
- Study says actual number of Covid-19 cases is far greater than thought, CNN, 7/21/2020 (Commentary)
- Bill Gates CBSN interview at-a-glance: Bill Gates on Coronavirus Vaccine Trials; Vaccine Side Effects, CBS-TV, 7/23/2020
- Pets show antibodies to SARS-CoV-2 in Italian study, Medical Life Sciences News, 7/24/2020
- Two American coronavirus vaccines from Moderna and Pfizer begin the last phase of testing: 30,000-person trials, Washington Post, 7/27/2020 (Commentary)
- How to Hold Beijing Accountable for the Coronavirus, Wall Street Journal, 7/28/2020
- Old Vaccines May Stop the Coronavirus, Study Hints. Scientists Are Skeptical, New York Times, 7/29/2020
- Dozens of COVID-19 vaccines are in development. Here are the ones to follow, National Geographic, 7/31/2020 (Commentary)
- China’s coronavirus vaccines face hurdles, Nature, 7/31/2020
- Russia plans mass vaccinations by October, doctors and teachers will be first, health officials said, FOX News, 8/1/2020 (Commentary)
- Russia gears up for mass vaccination against coronavirus despite international skepticism, CNBC, 8/3/2020
- Nearly 1.5 million people in Italy have coronavirus antibodies: study, Local IT, 8/4/2020
- Sweden’s top virologist has a message on how to defeat coronavirus: Open schools and no masks, Fortune, 8/5/2020 (Commentary)
- Children and the virus: As schools reopen, much remains unknown about the risk to kids and the peril they pose to others, Washington Post, 8/10/2020
- Why does COVID-19 strike some and not others? Fauci sees an answer in new study, Miami Herald, 8/11/2020
- A mathematical model reveals the influence of population heterogeneity on herd immunity to SARS-CoV-2, Science, 8/14/2020
- Russia produces first batch of COVID-19 vaccine: Interfax, Reuters, 8/15/2020
 |
July 14, 2020 – World’s first recorded case of a child contracting COVID-19 from its mother inside the womb, Business Insider
Business Insider reports that Doctors in France have reported what they say is the first confirmed case of a child contracting the coronavirus from their mother while still in the womb.
The case was the subject of a paper titled “Transplacental transmission of SARS-CoV-2 infection,” published Tuesday in the peer-reviewed journal Nature Communications. Details of the paper were first reported by The Guardian.
Until now, there has been limited evidence suggesting that a child could catch the coronavirus from inside the womb, but the paper’s authors, from the Antoine Béclère hospital, in Paris, confirmed “transplacental transmission of SARS-CoV-2” was possible.
They said a 23-year-old woman was admitted to the hospital with a fever and cough on March 24 when she was more than 35 weeks pregnant with a boy.
The mother tested positive for the coronavirus, gave birth by cesarean section, and the baby was immediately taken to the natal intensive care unit.
The baby tested positive for the virus. He later recovered and was discharged 18 days later, the doctors said.
They said the baby’s brain bore evidence of inflammation caused by the coronavirus, which had crossed the placenta into the baby’s bloodstream.
They ruled out the chance that the baby caught the virus after birth by viral or bacterial means.
“The placenta showed signs of acute and chronic intervillous inflammation consistent with the severe systemic maternal inflammatory status triggered by SARS-CoV-2 infection,” the authors said.
 |
July 14, 2020 – A Look at the Coronavirus Reinfection Rate, National Review
National Review reported that yesterday brought two stories that seemed like just about the worst news we could get in this pandemic. First, the Guardian over in the U.K. reported on a study by King’s College London suggesting that after infection, coronavirus patients could lose their built-in immunity to reinfection fairly quickly:
Blood tests revealed that while 60 percent of people marshalled a “potent” antibody response at the height of their battle with the virus, only 17 percent retained the same potency three months later. Antibody levels fell as much as 23-fold over the period. In some cases, they became undetectable.
“People are producing a reasonable antibody response to the virus, but it’s waning over a short period of time and depending on how high your peak is, that determines how long the antibodies are staying around,” said Dr Katie Doores, lead author on the study at King’s College London.
Then, over in Vox, D. Clay Ackerly, an internal medicine and primary-care physician practicing in Washington, D.C., described a 50-year-old patient who tested positive, suffered the effects, tested negative twice, then tested positive again with more severe symptoms a second time, about six weeks later:
It is possible, but unlikely, that my patient had a single infection that lasted three months. Some Covid-19 patients (now dubbed “long haulers”) do appear to suffer persistent infections and symptoms.
I believe it is far more likely that my patient fully recovered from his first infection, then caught Covid-19 a second time after being exposed to a young adult family member with the virus. He was unable to get an antibody test after his first infection, so we do not know whether his immune system mounted an effective antibody response or not.
We’ve had these worries earlier this year. Back in early April, South Korean doctors initially believed they were seeing people get sick a second time from “reactivation” of the virus. The Korean CDC initially characterized these cases as “reactivation” of the virus, not reinfection, believing the body fights off the virus for a while, at a sufficient level to make the virus seem dormant, and then the immune system stops fighting it as effectively, causing a second flare-up.
But by the end of the month, the South Korean CDC concluded the patients tested positive a second time “because fragments of the virus remained in their bodies and showed up in test kits.” Apparently, the tests the South Koreans were using were “so sensitive that [they] can still pick up parts of the small amount of RNA from a cell even after the person has recovered from COVID-19.”
An earlier antibody test on Dr. Ackerly’s patient would have been particularly useful in unraveling this mystery. Maybe the patient’s body exhibited something similar to the original South Korean theory — his body fought off almost all of the virus but not quite all of it, enough to test negative. (We should also recognize that some small portion of tests will give inaccurate results. If the tests are 90 percent accurate, wouldn’t one patient out of 100 positive patients generate two false negatives in a row?) With the virus mostly but not entirely gone, the patient’s immune system “relaxes”. . . and eventually, the virus returns with a vengeance, worse the second time because the viruses that survived the first battle are a little tougher and the ones that are best adapted to fight the patient’s immune system.
Or maybe this patient’s immune system is just not that strong. As noted yesterday, a lot of how our body responds to pathogens is determined by our genes, and some human beings hit the jackpot and have immunity or near-immunity to some common health problems. (A small minority of humans are immune to mosquito bites.) In the eyes of the patient, the difference between “reinfection” and “reactivation” is probably moot; in either case, you get sick, you get better, you think you’re in the clear, and then you get sick again.
It is also theoretically possible that this patient encountered a mutated strain of the coronavirus that is too different from the first strain for his body to effectively fight it off. Before you start worrying about that, keep in mind that so far, the only significant mutation of SARS-CoV-2 that researchers have uncovered is one that makes it more contagious, not more deadly or too different for a patient’s immune system to recognize. (Some scientists think the virus might be getting less deadly, but the jury is still out on that, so to speak. A declining rate of death among the infected, like we’re seeing right now, might be because the virus is growing less virulent, but it’s difficult to differentiate that factor from the improvements in treatment and less vulnerable patients getting infected in the current waves.)
As Ed Cara notes, the body’s response to a viral infection utilizes both antibodies and T-cells, which you may have heard of in the context of cancer treatments. T-cells are produced in bone marrow but get their name because they develop in the thymus gland. T-cells are basically the special forces of your immune system and split into two groups. The first, CD8, acts as the Navy SEALS of your immune system: They take on infections, virus bacteria, and tumors and, God willing, take them all down. The second category of T-cells, CD4, are the support staff, performing a variety of duties . . . including the production of cytokines. (Readers who remember past articles about chloroquine and hydroxychloroquine recognize that term from the discussion of the dangers of “cytokine storms” and how that drug can prevent the immune system from overreacting at attacking healthy cells.) Our bodies’ production of T-cells slows after puberty and basically is gone by age 65, which is one reason why elderly people are more vulnerable to infection.
As this Wired article lays out, some new research suggests that bodies with not-so-great antibody levels can still have effective T-cell responses against this virus. The study found SARS-CoV-2-specific CD8 T-cells were found in about 70 percent of recovering patients and 100 percent of patients had CoV-2-specific CD4 T-cells. But also, “importantly, we detected SARS-CoV-2-reactive CD4+ T cells in ∼40 percent –60 percent of unexposed individuals, suggesting cross-reactive T cell recognition between circulating ‘common cold’ coronaviruses and SARS-CoV-2.”
“Do not fear the (coronavirus) wolf. The wolf will make us strong and clean… The wolf is preparing people for greatness again.” — Bruce Brown
In other words, 40 to 60 percent of people who hadn’t caught the virus yet had T-cells that had been “in training” against regular non-SARS-CoV-2 coronaviruses and that were likely to be effective in fighting off SARS-CoV-2. (Suddenly, asymptomatic cases make a bit more sense. Those folks are probably lucky enough to have immune systems that are top-tier and never let the SARS-CoV-2 virus get enough traction to generate symptoms. Remember, coughs, sneezes, runny noses, and other symptoms of sickness are ways the body is trying to expel the invader.)
The body’s immunity against reinfection from other types of coronaviruses is pretty impressive. Keep in mind: Most of the common colds are coronaviruses; if our bodies couldn’t retain the ability to fight them off, we would keep catching the same cold over and over again throughout the winter. One study of seven Jordanians infected with MERS — Middle East Respiratory System — found that six had antibodies in their system nearly three years later. (That sample may seem small, but remember MERS only infected about 2,500 people total.)
Is Herd Immunity Still Far, Far Away . . . or Closer Than Most People Think?
Last night, Mississippi governor Tate Reeves offered a clear and succinct series of tweets, laying out why he’s not putting too much hope in “herd immunity” taking effect in his state. He noted that just to reach the threshold of 40 percent infected, the number of infected in his state would have to increase from the roughly 37,000 known infections to about 1.2 million. Are there asymptomatic people walking around Mississippi, unaware they have the virus? Sure. Are there 100,000? Half a million? A million?
Reeves summarizes, “on our worst day of new cases, we had just over 1,000. It has typically been between 700-900 during this most aggressive time. To get to 40% infections, we’d need 3,187 new cases every day for a full year from today. We would need to TRIPLE our worst day — every day — for a year.”
With that said, it is reasonable to believe that certain neighborhoods and communities that were particularly hard hit in the early stages of this pandemic might have reached herd immunity, or something close to it. A of couple days ago, the New York Times reported, “At a clinic in Corona, a working-class neighborhood in Queens, more than 68 percent of people tested positive for antibodies to the new coronavirus. At another clinic in Jackson Heights, Queens, that number was 56 percent. But at a clinic in Cobble Hill, a mostly white and wealthy neighborhood in Brooklyn, only 13 percent of people tested positive for antibodies.” The article cautiously notes that the people who come into the clinic to be tested may not be representative of the neighborhoods as a whole.
New York political leaders are particularly pleased with the declining number of deaths and new cases these days. Yes, this is what happens when the virus has burned through an area so thoroughly — the virus finds fewer and fewer people who don’t have the antibodies.
 |
July 14, 2020 – Florida tops its single-day record for coronavirus deaths, but death rate falls through floor to less than 1%, Chicago Tribune (Commentary)
The Chicago Tribune reports that Florida surpassed its daily record for coronavirus deaths Tuesday amid rising global worries of a resurgence.
Florida’s 132 additional deaths topped a state mark set just last week. The figure likely includes deaths from the past weekend that had not been previously reported.
The new deaths raised the state’s seven-day average to 81 per day, more than double the figure of two weeks ago and now the second-highest in the United States behind Texas.
The worrisome figures were released just hours before the news about the experimental vaccine, developed by the National Institutes of Health and Moderna Inc.
With the virus spreading quickly in the southern and western U.S., one of the country’s top public health officials offered conflicting theories about what is driving the outbreak.
“We tried to give states guidance on how to reopen safely. …If you look critically, few states actually followed that guidance,” Dr. Robert Redfield, the director of the Centers for Disease Control and Prevention said Tuesday in a livestream interview with the editor of the Journal of the American Medical Association.
Redfield said people in many states did not adopt social distancing and other measures because they hadn’t previously experienced an outbreak. But he went on to say, without explanation, that he didn’t believe the way those states handled reopening was necessarily behind the explosive rise in virus cases. He offered a theory that infected travelers from elsewhere in the country might have brought the virus with them around Memorial Day.
CDC officials said that there are various possible explanations, and that Redfield was offering just one.
Doctors in Florida have predicted more deaths as daily reported cases have surged from about 2,000 a day a month ago to a daily average of about 11,000, including a record 15,000 on Sunday. The state recorded 9,194 new cases Tuesday.
Marlyn Hoilette, a nurse who spent four months working in the COVID-19 unit of her Florida hospital until testing positive recently, said hospitals are so desperate for staff to return to work they are not following guidelines that call for two negative tests first.
“Nurses are getting sick, nursing assistants are getting sick and my biggest fear is that it seems we want to return folks to work even without a negative test,” said Hoilette, who works at Palms West Hospital in Loxahatchee. Florida. “It’s just a matter of time before you wipe the other staff out if you’re contagious, so that is a big problem.”
Commentary — you can smell the hysteria in this story — and the hospital staff crisis in Florida appears to be real, as it is everywhere in the U.S. — but the plain fact of the matter is that the Florida daily death toll from coronavirus — while setting a record — is actually not huge.
We’re looking at a record 132 deaths a day in Florida compared to a record 15,300 new cases a day in Florida. That’s a mortality rate of on the record day of .8 percent, or less than 1 percent.
This figure is supported by a recent New York Times story, which reported that COVID-19 is now believed to have a mortality rate of a little better than 1/2 of 1 percent, meaning one person in every 200 who catches it may be expected to die from it, statistically speaking.
 |
July 14, 2020 — An mRNA Vaccine against SARS-CoV-2 — Preliminary Report, New England Journal of Medicine
A preliminary report in the New England Journal of Medicine states that 100% of one group of Moderna Vaccine Participants Suffered Side Effects in coronavirus vaccine trials ongoing right now.
The Moderna COVID-19 vaccine candidate (currently known only as mRNA-1273), was recently found to cause systemic side effects in 80% of Phase 1 participants receiving the 100 microgram (mcg) dose.
Side effects ranged from fatigue (80%), chills (80%), headache (60%) and myalgia or muscle pain (53%). After the second dose, 100% of participants in the 100-mcg group experienced side effects.
In the highest dosage group, which received 250 mcg, 100% of participants suffered side effects after both the first and second doses.3 Three of the 14 participants (21%) in the 250-mcg group suffered “one or more severe events.”
Despite these worrisome results, the trial is being heralded as a big success, and vaccine expert Dr. Paul Offit has been quoted in the American Reporter as saying we now know “that it’s safe in 45 people,” and that “it doesn’t have a very common side effect problem.”
Commentary — Thanks to Dr. Joseph Mercola at Mercola.com for the tip on the New England Journal of Medicine Story.
 |
June 15, 2020 – How a False Hydroxychloroquine Narrative Was Created, Mercola.com (Commentary)
Dr. Joseph Mercola of Mercola.com details how hydroxychloroquine — a cheap generic drug that has been used successfully against malaria for over half a century, and has recently been used successfully worldwide against COVID-19 — was demonized by the World Health Organization and the British medical publication The Lancet after it was touted by President Donald Trump (although Mercola does not mention Trump once in his article).
Mercola outlines how a WHO study partially funded by the Bill and Melinda Gates Foundation used lethal doses of hydroxychloroquine (“2,400 mg of hydroxychloroquine during the first 24 hours — three to six times higher than the daily dosage recommended”), and then concluded the drug — which has been used safely for decades — was unsafe, and how a study of hydroxychloroquine published in The Lancet — which also dubbed hydroxychloroquine unsafe — had to be quickly retracted for using fabricated data.
Commentary — This is a detailed, highly medical/scientific article which is hard to read, but also important — not just to the political debate in the United States, but also to the treatment of millions of people worldwide who are suffering from COVID-19.
As French science-prize winning microbiologist and infectious disease expert Dr. Didier Raoult, who is also founder and director of the research hospital Institut Hospitalo-Universitaire Méditerranée Infection, said on July 2, 2020, failure to prescribe hydroxychloroquine to a COVID-19 patient “should be grounds for malpractice.”
Yet the mud thrown at hydroxychloroquine and Trump by the WHO and The Lancet has stuck to a considerable degree in the minds of many Americans, especially liberals who reflexively believe anything negative about the President of the United States, and anything that swells the coffers of Big Pharma.
 |
July 15, 2020 – Your Ancestors Knew Death in Ways You Never Will, New York Times (Commentary)
The New York Times writes that some people say we’re doomed. But science and public spending have saved us from pandemics worse than this one.
Nearly 140,000 Americans have been lost to coronavirus, and many experts fear that the deaths will only accelerate in the fall as cold weather forces us indoors. By year’s end, half as many Americans may have died as did in the four years of World War II.
And yet we are still arguing over how to prevent this — each state struggling over how much lockdown to impose and what its governor can make its citizens do.
“You know the five stages of grief — denial, anger, bargaining, depression, acceptance?” asked Dr. Emily Landon, a coronavirus expert at the University of Chicago medical school. “I think the American people are in all five of them — but different parts of the country are in different stages.”
As death stalks us, especially our elders, have we simply become inured to the idea that many of us are doomed?
The stock market appears to have priced in a huge wave of deaths. In the 2008-2009 recession, it fell 50 percent and took four years to recover. In March it fell only 34 percent and has made up much of that ground already. Looked at with Wall Street’s bloodless arithmetic, that makes sense: Most of the deaths are among the very elderly and nursing home residents, who no longer travel or dine out or contribute much to the economy, and who are a burden on the struggling Medicare and Social Security Trust Funds.
One can even argue that the acceptance of death as master of us all is part of the human psyche. But because of modern medicine, we have been out of touch with our ultimate fate for generations.
We’ve all heard of the Black Death and perhaps the Plague of Justinian, events that may have killed up to a third of mankind and rewrote the fates of empires. They seem lost in the mists of time.
But not that long back, our great-great-great-great-grandparents felt the omnipresence of death in ways we will never know.
There is a chart famous among epidemiologists titled “The Conquest of Pestilence in New York City.” Produced by New York City’s health department, it tracks and explains deaths in the city from the early 1800s to the present day.
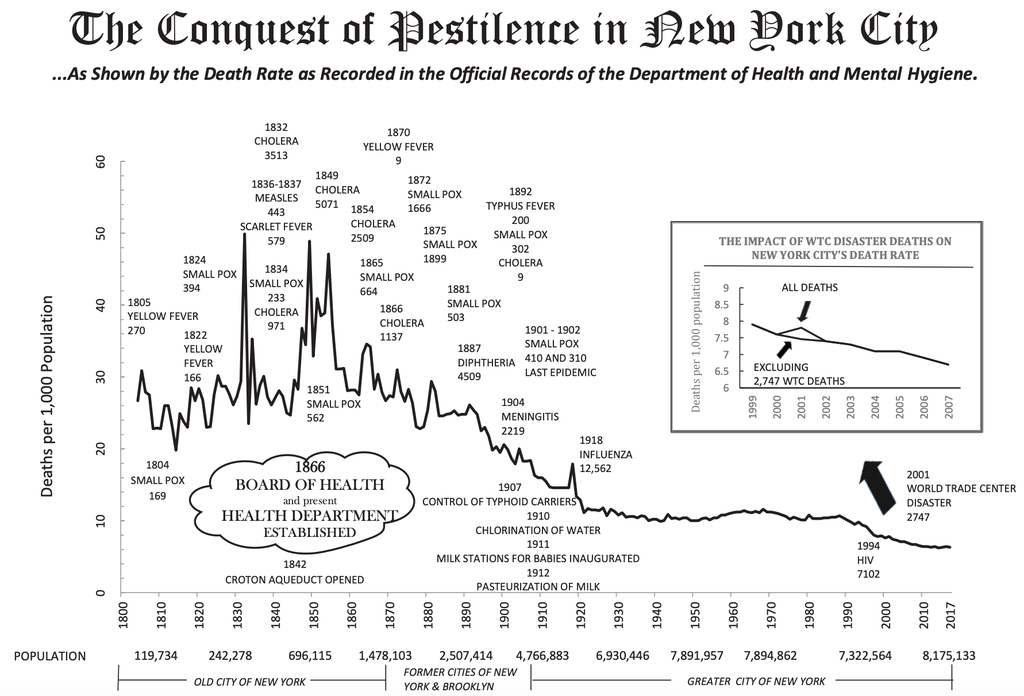
At first glance, it looks innocuous, like the ups and downs of the Dow Jones index. But the longer you stare at the fine print, the more horrified you become.
This past March, before coronavirus cases began to mount, the annual death rate in New York City was about six per 1,000 New Yorkers. The virus’s first wave added about 2.5 more deaths per 1,000 to that baseline. By contrast, from 1800 into the 1850s, deaths in the city rose in a relentless series of epidemic spikes, year after year, with only brief respites in between.
The annual baseline back then was about 25 deaths per 1,000 New Yorkers, and in some years the toll reached 50 per 1,000. In other words, in bad years, New Yorkers saw twice as many people around them die as usual. And they were used to seeing about four times as much death as we now do.
The sharpest peaks were the cholera epidemics of 1832, 1849 and 1854. But plagues came in waves, sometimes more than one simultaneously: yellow fever, smallpox, measles, scarlet fever, diphtheria, typhus and meningitis.
Other than cholera and typhus, most of those were childhood diseases that adults were immune to because they had survived them, so the chart is a parabola of parental grief, each spike another nail in a hundred small coffins.
The death rate began dropping after the 1860s. New Yorkers — both citizens and doctors — had finally stopped arguing and reached consensus on some basic issues.
First of all, most finally accepted the “germ theory” of disease, acknowledging that it was caused by invisible enemies, not by swamps, trash, manure or the other nuisances that underlay the “miasma theory,” which held that bad smells caused disease. (Only a century earlier, Americans had given up on the “humors theory,” which posited that disease was caused by imbalances among blood, urine, sweat and bile that had to be rebalanced by bleeding, sweating or purging.)
They also agreed that whether immigrants had brought some diseases or simply suffered from them, no one was safe until everyone was safe, so they made public health universal.
As a result, New Yorkers took certain steps — sometimes very expensive and contentious, but all based on science: They dug sewers to pipe filth into the Hudson and East Rivers instead of letting it pool in the streets. In 1842, they built the Croton Aqueduct to carry fresh water to Manhattan. In 1910, they chlorinated its water to kill more germs. In 1912, they began requiring dairies to heat their milk because a Frenchman named Louis Pasteur had shown that doing so spared children from tuberculosis. Over time, they made smallpox vaccination mandatory.
Libertarians battled almost every step. Some fought sewers and water mains being dug through their properties, arguing that they owned perfectly good wells and cesspools. Some refused smallpox vaccines until the Supreme Court put an end to that in 1905, in Jacobson v. Massachusetts.
In the Spanish flu epidemic of 1918, many New Yorkers donned masks but 4,000 San Franciscans formed an Anti-Mask League. (The city’s mayor, James Rolph, was fined $50 for flouting his own health department’s mask order.) Slowly, science prevailed, and death rates went down.
Today, Americans are facing the same choice our ancestors did: We can listen to scientists and spend money to save lives, or we can watch our neighbors die.
“The people who say ‘Let her rip, let’s go for herd immunity’ — that’s just public-health nihilism,” said Dr. Joia S. Mukherjee, the chief medical office of Partners in Health, a medical charity fighting the virus. “How many deaths do we have to accept to get there?”
A vaccine may be close at hand, and so may treatments like monoclonal antibodies that will cut our losses.
Till then, we need not accept death as our overlord — we can simply hang on and outlast him.
Commentary — THIS IS A silly and slight “think piece” that inadvertently reveals several things it does not intend or comprehend.
The first is how much the belief system of secular liberals resembles the belief system of Christian conservatives.
Both secular liberals — for whom the New York Times is frequently taken as a sort of Holy Book of Truth — and devout Christian conservatives believe humanity will be saved from this great coronavirus crisis by a higher, external force outside their everyday lives.
For Christians, it is the hand of almighty God. For secularists, it is the hand of almighty Science.
So the author of this piece (“Your Ancestors Knew Death in Ways You Never Will”), Donald G. McNeil Jr., contends that “science and public spending have saved us from pandemics worse than this one,” and it will save the day this time too. Although certainly comfortable enough as platitudes go, this statement is simply not true, nor does McNeil understand what “saved us” from past pandemics.
Here’s the matter of pandemics put simply. Every single pandemic that has afflicted the human species — from before the beginning of recorded history until now — has been been overcome and ended by a very simple behavioral and biological processes that are evident every day in the lives of human beings everywhere, and many other higher species on Earth as well.
These simple, every day processes produce cultural behavior and aggregate genetic movement toward what we now call “herd immunity,” meaning sufficient immunological resistance to a given microbial attacker so that the population is no longer susceptible to wildfire-like pandemics.
True, both religion and science can play a supporting role in the natural movement toward herd immunity. Religion can give people emotional strength, which is important because people’s emotions play such an big role in every struggle they face. And science likewise can play an important supporting role, especially if a vaccine can be created, since a vaccine can accelerate the species’ movement toward herd immunity, and save lives that would otherwise be lost in what remains a bitter battle to achieve herd immunity against COVID-19.
But neither religion nor science is the prime mover or the root cause here. The process that ends pandemics is natural, is with us every day, and has been with us as long as there have been human beings on earth. This is something that should make people everywhere on the earth feel good about our prospects in the battles to come, and proud and easy in their humanity .
The process has three parts — (1) the natural physical development of immunity through antibodies, T-Cells, immune system “dark matter,” and the other known and unknown natural processes of our physical bodies that fight invasive, infectious diseases, and (2) broad but not universal changes in human behavior (the species always hedges its bets) that increase herd immunity, and (3) the death of the weakest members of the populations who are tinder for the pandemic firestorm.
So a society with many weak members, and nursing homes full of the elderly, the injured and the brain dead, America was primed for a pandemic as 2020 dawned. It was like a dry California forest in the summer with a lot of dry dead branches and assorting underbrush lying on the ground because management authorities stopped the natural burning process, and created super fires for their trouble — the forest fire equivalent of a pandemic.
A profound irony of pandemics is that they make the human species strong and vital — physically, emotionally and intellectually. We — human beings as a species– will be a stronger, more competitively capable species when this pandemic is over than we are now.
Coronavirus is like the wolf packs that used to clean the once vast caribou herds of the Far North and keep them strong by killing the weak.
LET’S TAKE A look at New York plagues of the past, and the number of people they killed. These are plagues that this Times editorial says have been ended by “science and public spending.” Among others, we find the:
- Yellow fever epidemic of 1805, 270 people died in New York
- Small pox epidemic of 1824, 394 people died in New York
- Cholera epidemic of 1834, 3,053 people died in New York
- Cholera epidemic of 1854, 5,071 people died in New York
- Diptheria epidemic of 1887, 4,509 people died in New York
- Meningitis epidemic of 1904, 2,219 people died in New York
- Spanish influenza epidemic of 1918, 12,562 people died in New York
There were no vaccines for any of these diseases at the time of the New York epidemics listed above, so each of them flared and then burned through America’s largest city for as long as long and hard as herd immunity would let them, and they finally burned out as a super fire when easy or weak victims had been killed, and selectively eliminated.
Changes in human behavior during plagues frequently affect herd immunity for the species too, both for and against. In A Journal of the Plague Year, Daniel Defoe (of Treasure Island fame) describes how residents of London became highly concerned with the cleanness of the air they breathed with others during the Plague of 1665 (just like with COVID-19 today), so they fled the cities (just like with COVID-19 today), thereby spreading the plague to remote areas outside the cities (just like with COVID-19 today).
Defoe also describes what we today call asymptomatic carriers:
“I mean such as had received the contagion, and had it really upon them, and in their blood, yet did not show the consequences of it in their countenances: nay, even were not sensible of it themselves, as many were not for several days. These breathed death in every place, and upon everybody who came near them; nay, their very clothes retained the infection, their hands would infect the things they touched, especially if they were warm and sweaty, and they were generally apt to sweat too.
Now it was impossible to know these people, nor did they sometimes, as I have said, know themselves to be infected…
Defoe also describes increasingly stringent but not always effectual laws enacted by the City of London to try to stop the spread of the contagion (just like with COVID-19 today). Londoners in 1665 were fully alive to the threat of airborne, aerosol infection, just people are today with the COVID-19 masks that many people are required to wear now. In 1665, Defoe wrote of how the Bubonic plague spread by “mutual respiration”:
Contagion is the inseparable symptom of the plague; which, by mutual respiration, is transfused from the infected persons to the lungs and stomach of those who approach them.
AND THERE ARE also echoes of what we’re experiencing today in the annals of the ancient world. During the so-called Justinian plague that struck Europe in 541 AD, during the reign of Roman Emperor Justinian, the functioning of the Roman Empire was significantly disrupted by the Bubonic plague, Yersinia pestis. Justinian himself was sickened, but recovered. Modern medical research has established that the strain of Bubonic plague that wasted the last years of Justinian’s reign had originated in China (just like with COVID-19 today).
And nearly a millennia before Justinian, Greek philosopher Socrates was said by Edward Gibbon in The Decline and Fall of the Roman Empire to have lived through the plague that struck Athens during the second year of the Peloponnesian War (430 BC) by virtue of his “temperance.”
Ancient Greek physicians argued about whether a recovered plague patient could be reinfected with the plague — in other words, whether plague survivors achieved strong immunity against re-infection (just like with COVID-19 today). Thucydides argued that plague survivors acquired immunity, while Gibbons wrote that “Evagrius, who had family experience of the plague, observes, that some persons, who had escaped the first, sunk under the second attack; and this repetition is confirmed by Fabius Paullinus.”
THE ONLY REASON I mention all this is to demonstrate that the chaotic behavior we’ve seen in the global reaction to the COVID-19 pandemic during it’s first six months is just fine.
So you say the government didn’t get a good handle on the situation at the outset, when it could have made a big difference? Don’t worry about it. It’s scripted that way, and that’s exactly how human pandemic dramas have played out, over and over again.
THIS IS HOW HUMAN BEINGS ACT WHEN A PANDEMIC CONFRONTS THEM. It’s been going on for thousands of years beyond counting. It’s how we get the job done, as a species. It’s how we survive.
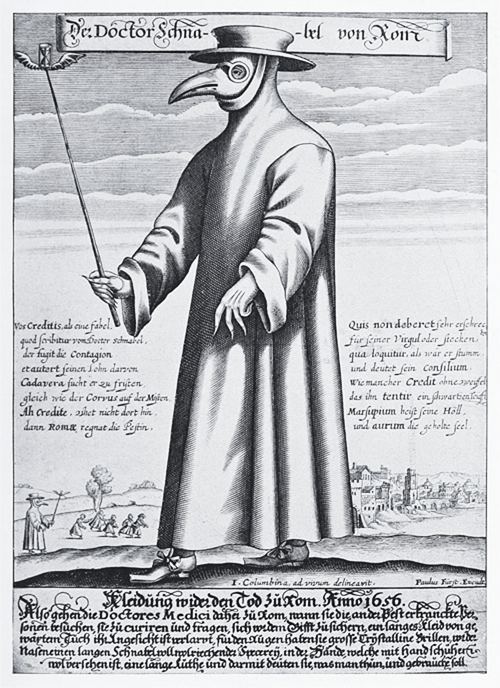
Please note, however. There was never a vaccine against any of these ancient plagues of ancient Greece and Rome, as there was no vaccine for Defoe’s London plague of 1665, which is also the plague that produced Der Doctor Schnabel von Rom (“Doctor Nose of Rome”).
Science as we know it today did not even exist, and was not a factor at all in these stories. Here, the natural bio/behavioral process of creating herd immunity overcame every plague threat naturally.
Sometimes the human cost of combing out the weak undercoat of humanity was considerable, and authentically tragic. But the species has come through every single plague threat it has ever faced, and come through stronger. As with the arctic caribou and the wolf, we do better as a species when our weakness is combed out.
FINALLY, I must concede that New York Times science reporter Donald G. McNeil Jr. is correct in one respect — public spending has played a role in the history of human plagues.
In Defoe’s time, the City of London and other afflicted cities of Europe undertook modest public expenditures to control the disease’s spread, which began with burying the dead, a public minded act that immediately increased taxes since the citizens of London were levied a burial tax to pay for the monthly public expenditures to bury the dead.
The City of London’s next recourse, according to Defoe, was to lock anyone diagnosed with the plague and their entire family in one house together under lock and guard, which could amount to a death sentence for anyone diagnosed and anyone they had contact with, when it was strictly enforced, which it sometimes was.
A thousand years before, in the nearly decade long era of the Justinian plague, the Romans still had the scope and power to levy and expend in quantities that might meet a stricter definition of “public expenditure.” And Emperor Justinian did expend, although mostly for bureaucracy to try to maintain the pre-plague tax flow to Imperial coffers, so that — according to the Gibbon — the living were liable for their own tax obligation, as well as the tax obligation of their plague deceased neighbors.
And yet the human species survived, thrived, conquered new and unimagined realms like never before. So there’s no need to fear the wolf, which for us is coronavirus.
We need the wolf to make us strong and successful, and I’ll say it again — we are going to come out of this pandemic a stronger species than we were going in.
 |
July 16, 2020 – The coronavirus pandemic most resembles the the 1957 Asian flu pandemic, Coronavirus Vaccine & Herd Immunity Digest
The Coronavirus Vaccine & Herd Immunity Digest writes that the coronavirus pandemic has most frequently been compared to the 1919 Spanish influenza pandemic, which was the most deadly flu epidemic in history.
The CDC estimates that 675,000 people died from the Spanish influenza in the United States, and a 2006 CDC article says the Spanish influenza’s case fatality rate was around 2.5%, which means 2.5 percent of people infected died, although both the death rate and the total number of deaths may have been much higher.
By comparison, there have been 138,000 death attributed to COVID-19 to date, and the COVID-19 mortality rate was recently calculated by the New York Times at 0.6 percent, or about 1/2 or 1 percent, meaning 1/2 of 1 percent of those infected may be expected to die.
So both the total death count and the death rate attributed to the coronavirus pandemic are far, far lower than those observed with the Spanish influenza, which was a more potent killer than COVID-19 by all measures.
What then can COVID-19 be meaningfully compared to? How about the Asian flu?
Both the coronavirus and the Asian flu are novel coronaviruses which apparently crossed over to humans from non-human species. In the case of the Asian flu, the origin was the H2N2 avian flu (possibly from geese), and both pandemics came out of China. The Asian flu first appeared in Guizhou, China, in late 1956, then in Singapore and Hong Kong in the spring of 1957.
In terms of mortality rate, the COVID-19 and Asian flu pandemics are very similar. Like COVID-19, the Asian flu had a human mortality rate of a little more than 1/2 of 1 percent. “The case fatality rate of Asian flu was approximately 0.67%,” according to Wikipedia.
The estimated number deaths attributed to the Asian flu and coronavirus are somewhat comparable as well. There were 116,000 Asian flu deaths in the United States, according to the CDC, compared to 138,000 deaths from COVID-19 in the U.S. to date. (Because the population of the Unites States was much smaller in 1957, the Asian flu actually killed a larger percentage of the American population than COVID-19 has so far.)
And like COVID-19, the Asian flu hit the elderly hardest and was most deadly for that portion of the population.
There are, however, two big differences between the Asian flu and COVID-19 stories. The first is that the U.S. was able to have a vaccine ready by the fall of 1957, when the Asian flu hit America.
The other difference is that no one gave even a moment’s thought to closing the whole country down for the Asian flu pandemic, even though its mortality rate and death count were similar to the coronavirus pandemic.
There was no heavy-breathing hysteria in America in 1957. People just took the best precautions they could, and got on with it.
 |
July 17, 2020 – Nobel Laureate Calls COVID-19 Manmade, Cnews (Commentary)
French virologist Luc Antoine Montagnier, who was awarded a Nobel prize in Physiology in 2008 along with Françoise Barré-Sinoussi and Harald zur Hausen for discovering of the HIV virus, says COVID-19 is manmade.
Appearing on the French cable TV show, CNews, on April 17, 2020, Luc Antoine Montagnier stated that the virus that causes COVID-19 is manmade, and that elements of HIV and Plasmodium falciparum, a parasite that causes malaria, are found in the coronavirus’s genome.
Montagnier said:
“We were not the first since a group of Indian researchers tried to publish a study which showed that the complete genome of this coronavirus [has] sequences of another virus, which is HIV.”
The research that Montagnier refers to was posted on the science website Biorxiv January 31, 2020, and has since been withdrawn. The Indian researchers wrote:
“We found 4 insertions in the spike glycoprotein (S) which are unique to the 2019-nCoV and are not present in other coronaviruses. Importantly, amino acid residues in all the 4 inserts have identity or similarity to those in the HIV-1 gp120 or HIV-1 Gag …
The finding of 4 unique inserts in the 2019-nCoV, all of which have identity /similarity to amino acid residues in key structural proteins of HIV-1 is unlikely to be fortuitous in nature.”
Montagnier says COVID-19 Derives From a Failed HIV Vaccine.
In a separate appearance on the French podcast Pourquoi Docteur, also April 17, Montagnier said the coronavirus had escaped in an “industrial accident” while Chinese scientists at the Wuhan city laboratory were trying to develop a vaccine against HIV. “In order to insert an HIV sequence into this genome, molecular tools are needed, and that can only be done in a laboratory,” said Montagnier.
Montagnier also said he believes that the pandemic will naturally extinguish itself because of its synthetic origins:
“Nature does not accept any molecular tinkering, it will eliminate these unnatural changes and even if nothing is done, things will get better, but unfortunately after many deaths.”
According to the website Corvelva, Montagnier said on the podcast that the pandemic would peter out because nature would override the synthetically inserted sequences that make COVID-19 so deadly:
Montagnier says he reached his conclusions, “With my colleague, biomathematician Jean-Claude Perez,” after they “carefully analyzed the description of the genome of this RNA virus.” Montagnier’s partner, Perez, is a French interdisciplinary scientist and biomathematics expert.
In a paper Montagnier and Perez published by the Center for Open Science in April 2020, they write:
“Using our proprietary bio-mathematic approach we are able to evaluate the level of cohesion and organization of a genome; … we then searched in this genome for possible traces of HIV or even SIV [related simian immunodeficiency virus]. A first publication reports the discovery of 6 HIV SIV RNA pieces.”
The HIV and SIV elements that Montagnier and Perez detect, called Exogenous Informative Elements, or EIEs, provide the basis of their theory that COVID-19 is not a simple derivative of SARS and bat-related viruses. They write:
“A major part of these 16 EIE already existed in the first SARS genomes as early as 2003. However, we demonstrate how and why a new region including 4 HIV1 HIV2 Exogenous Informative Elements radically distinguishes all COVID-19 strains from all SARS and Bat strains …
… a contiguous region representing 2.49% of the whole COVID-19 genome is 40.99% made up of 12 diverse EIE originating from various strains of HIV SIV retroviruses …
a novel long region of around 225 nucleotides, appears to us to be totally new: this region is completely absent in ALL SARS genomes, whereas it is present and 100% homologous for all COVID-19 genomes listed in NCBI or GISAID COVID_19 genomic databases.”
In June 2020, research published in the Quarterly Review of Biophysics makes similar claims. Norwegian scientist Birger Sørensen and British oncologist Angus Dalgleish refer to COVID-19 as a “chimeric virus” and write:
“We show the non-receptor dependent phagocytic general method of action to be specifically related to cumulative charge from inserted sections placed on the SARS-CoV-2 Spike surface in positions to bind efficiently by salt bridge formations; and from blasting the Spike we display the non human-like epitopes from which Biovacc-19 has been down-selected.”
While conceding the Quarterly Review of Biophysics assertions were controversial, the scientific website Minerva wrote that the science should be pursued.
“Minerva has read a draft of the article, and has after an overall assessment decided that the findings and arguments do deserve public debate, and that this discussion cannot depend entirely on the publication process of scientific journals.”
Commentary — if you’re wondering why you haven’t heard this before, the reason is that these highly significant comments by a distinguished scientist in the field have been completely ignored by the American press.
 |
July 18, 2020 – State Department releases cable that launched claims that coronavirus escaped from Chinese lab, Washington Post (Commentary)
The Washington Post reports that the U.S. State Department has released an internal cable from 2018 detailing the concerns of U.S. Embassy officials in China about a lack of adequately trained personnel at a virology lab in Wuhan, the city that later became the epicenter of the novel coronavirus outbreak.
Leaked contents of the cable sparked unproven speculation from senior U.S. officials beginning in April that the outbreak occurred as a result of an accident at the Wuhan Institute of Virology.
In May, President Trump said he had seen evidence that gave him a “high degree of confidence” that the coronavirus originated in a Chinese lab. When asked why he was confident, Trump said, “I can’t tell you that. I’m not allowed to tell you that.”
The full cable does not strengthen the claim that an accident at the lab caused the virus to escape, nor does it exclude the possibility. However, in recent months, skepticism of the accident theory has increased in the scientific community because the genetic sequences of isolates from the bat coronaviruses known to be under research at the lab do not match those of covid-19.
The State Department cable says the lab, which U.S. officials visited in 2018, “has a serious shortage of appropriately trained technicians and investigators needed to safely operate this high-containment laboratory.”
It also says that scientists in the lab were allowed to study SARS-like coronaviruses isolated from bats but were precluded from studying human-disease-causing SARS coronaviruses in their lab unless given explicit permission from a designated commission.
When asked on Friday whether he had evidence supporting the lab theory beyond the 2018 memo, a spokesperson did not point to a specific of piece of information but offered Pompeo’s remarks from Wednesday calling on China to be transparent.
“They have destroyed samples; they’ve taken journalists and doctors who were prepared to talk about this and not permitted them to do what nations that want to play on a truly global scale and global stage ought to do: be transparent and open and communicate and cooperate,” Pompeo said
The Office of the Director of National Intelligence has not endorsed or refuted the lab theory. In May, it issued a statement saying intelligence officials were still examining whether the virus “began through contact with infected animals or if it was the result of an accident at a laboratory in Wuhan.”
Commentary — There is a significant omission in this story which seriously slants it.
The Post states, “skepticism of the accident theory has increased in the scientific community because the genetic sequences of isolates from the bat coronaviruses known to be under research at the lab do not match those of covid-19.”
Is it possible that the Washington Post is unfamilar with the recent comments of distinguished French virologist Luc Antoine Montagnier? Montagnier, who was awarded a Nobel prize in Physiology in 2008 for his work identifying HIV, has said his research indicates that COVID-19 has been genetically engineered, and is manmade.
This comment from a highly respected scientist in the field not only lends credence to President Trump’s claim, it explains WHY the COVID-19 form of the virus doesn’t perfectly match Wuhan Lab sample RaTG13 — namely that COVID-19 has been genetically engineered from a naturally occuring coronavirus.
Furthermore, as the Times of London has reported, the Wuhan Institute of Virology (WIV) has acknowledged that it was performing “gain-of-function” genetic alterations on viruses to increase their virility, and make them more infectious to human beings. So we know that the Chinese were in fact performing genetic engineering on coronavirus specimens in their posession!
According to the Times of London:
This “gain-of-function” work is described in papers released by the WIV between 2015 and 2017, scientists say. Shi’s team combined snippets of different coronaviruses to see if they could be made more transmissible in what they called “virus infectivity experiments”.
Does the Washington Post think Nobel Laureate Luc Antoine Montagnier is not a member of the “scientific community”?! And is the Post unaware that the WIV was performing “gain-of-function” genetic engineering on the coronavirus specimens it had collected?!
Or maybe the Post is just willfully ignorant of these facts because they don’t fit its political agenda?
 |
July 19, 2020 — The people with hidden immunity against Covid-19, BBC
Zaria Gorvett of the BBC writes that while the latest research suggests that antibodies against Covid-19 could be lost in just three months, a new hope has appeared on the horizon: the enigmatic T cell.
The clues have been mounting for a while. First, scientists discovered patients who had recovered from infection with Covid-19, but mysteriously didn’t have any antibodies against it. Next it emerged that this might be the case for a significant number of people. Then came the finding that many of those who do develop antibodies seem to lose them again after just a few months.
In short, though antibodies have proved invaluable for tracking the spread of the pandemic, they might not have the leading role in immunity that we once thought. If we are going to acquire long-term protection, it looks increasingly like it might have to come from somewhere else.
But while the world has been preoccupied with antibodies, researchers have started to realise that there might be another form of immunity – one which, in some cases, has been lurking undetected in the body for years. An enigmatic type of white blood cell is gaining prominence. And though it hasn’t previously featured heavily in the public consciousness, it may well prove to be crucial in our fight against Covid-19. This could be the T cell’s big moment.
T cells are a kind of immune cell, whose main purpose is to identify and kill invading pathogens or infected cells. It does this using proteins on its surface, which can bind to proteins on the surface of these imposters. Each T cell is highly specific – there are trillions of possible versions of these surface proteins, which can each recognise a different target. Because T cells can hang around in the blood for years after an infection, they also contribute to the immune system’s “long-term memory” and allow it to mount a faster and more effective response when it’s exposed to an old foe.
Several studies have shown that people infected with Covid-19 tend to have T cells that can target the virus, regardless of whether they have experienced symptoms. So far, so normal. But scientists have also recently discovered that some people can test negative for antibodies against Covid-19 and positive for T cells that can identify the virus. This has led to suspicions that some level of immunity against the disease might be twice as common as was previously thought.
Most bizarrely of all, when researchers tested blood samples taken years before the pandemic started, they found T cells which were specifically tailored to detect proteins on the surface of Covid-19. This suggests that some people already had a pre-existing degree of resistance against the virus before it ever infected a human. And it appears to be surprisingly prevalent: 40-60% of unexposed individuals had these cells.
It looks increasingly like T cells might be a secret source of immunity to Covid-19.
The central role of T cells could also help to explain some of the quirks that have so far eluded understanding – from the dramatic escalation in risk that people face from the virus as they get older, to the mysterious discovery that it can destroy the spleen.
Deciphering the importance of T cells isn’t just a matter of academic curiosity. If scientists know which aspects of the immune system are the most important, they can direct their efforts to make vaccines and treatments that work.
How immunity unfolds
Most people probably haven’t thought about T cells, or T lymphocytes as they are also known, since school, but to see just how crucial they are for immunity, we can look to late-stage Aids. The persistent fevers. The sores. The fatigue. The weight loss. The rare cancers. The normally harmless microbes, such as the fungus Candida albicans – usually found on the skin – which start to take over the body.
Over the course of months or years, HIV enacts a kind of T cell genocide, in which it hunts them down, gets inside them and systematically makes them commit suicide. “It wipes out a large fraction of them,” says Adrian Hayday, an immunology professor at King’s College London and group leader at the Francis Crick Institute. “And so that really emphasises how incredibly important these cells are – and that antibodies alone are not going to get you through.”
During a normal immune response – to, let’s say, a flu virus – the first line of defence is the innate immune system, which involves white blood cells and chemical signals that raise the alarm. This initiates the production of antibodies, which kick in a few weeks later.
“And in parallel with that, starting out about four or five days after infection, you begin to see T cells getting activated, and indications they are specifically recognising cells infected with the virus,” says Hayday. These unlucky cells are then dispatched quickly and brutally – either directly by the T cells themselves, or by other parts of the immune system they recruit to do the unpleasant task for them – before the virus has a chance to turn them into factories that churn out more copies of itself.
The good and bad news
So, what do we know about T cells and Covid-19?
“Looking at Covid-19 patients – but also I’m happy to say, looking at individuals who have been infected but did not need hospitalisation – it’s absolutely clear that there are T cell responses,” says Hayday. “And almost certainly this is very good news for those who are interested in vaccines, because clearly we’re capable of making antibodies and making T cells that see the virus. That’s all good.”
In fact, one vaccine – developed by the University of Oxford – has already been shown to trigger the production of these cells, in addition to antibodies. It’s still too early to know how protective the response will be, but one member of the research group told BBC News that the results were “extremely promising”. (Read more about the Oxford University vaccine and what it’s like to be part of the trial).
There is a catch, however. In many patients who are hospitalised with more serious Covid-19, the T cell response hasn’t quite gone to plan.
“Vast numbers of T cells are being affected,” says Hayday. “And what is happening to them is a bit like a wedding party or a stag night gone wrong – I mean massive amounts of activity and proliferation, but the cells are also just disappearing from the blood.”
One theory is that these T cells are just being redirected to where they’re needed most, such as the lungs. But his team suspects that a lot of them are dying instead.
“Autopsies of Covid-19 patients are beginning to reveal what we call necrosis, which is a sort of rotting,” he says. This is particularly evident in the areas of the spleen and lymph glands where T cells normally live.
Disconcertingly, spleen necrosis is a hallmark of T cell disease, in which the immune cells themselves are attacked. “If you look in post-mortems of Aids patients, you see these same problems,” says Hayday. “But HIV is a virus that directly infects T cells, it knocks on the door and it gets in.” In contrast, there is currently no evidence that the Covid-19 virus is able to do this.
“There are potentially many explanations for this, but to my knowledge, nobody has one yet,” says Hayday. “We have no idea what is happening. There’s every evidence that the T cells can protect you, probably for many years. But when people get ill, the rug seems to be being pulled from under them in their attempts to set up that protective defence mechanism.”
Dwindling T cells might also be to blame for why the elderly are much more severely affected by Covid-19.
Hayday points to an experiment conducted in 2011, which involved exposing mice to a version of the virus that causes Sars. Previous research had shown that the virus – which is also a coronavirus and a close relative of Covid-19 – triggered the production of T cells, which were responsible for clearing the infection.
The follow-up study produced similar results, but the twist was that this time the mice were allowed to grow old. As they did so, their T cell responses became significantly weaker.
However, in the same experiment, the scientists also exposed mice to a flu virus. And in contrast to those infected with Covid-19, these mice managed to hold onto their T cells that acted against influenza well into their twilight years.
“It’s an attractive observation, in the sense that it could explain why older individuals are more susceptible to Covid-19,” says Hayday. “When you reach your 30s, you begin to really shrink your thymus [a gland located behind your sternum and between your lungs, which plays an important role in the development of immune cells] and your daily production of T cells is massively diminished.”
What does this mean for long-term immunity?
“With the original Sars virus [which emerged in 2002], people went back to patients and definitely found evidence for T cells some years after they these individuals were infected,” says Hayday. “This is again consistent with the idea that these individuals carried protective T cells, long after they had recovered.”
The fact that coronaviruses can lead to lasting T cells is what recently inspired scientists to check old blood samples taken from people between 2015 and 2018, to see if they would contain any that can recognise Covid-19. The fact that this was indeed the case has led to suggestions that their immune systems learnt to recognise it after being encountering cold viruses with the similar surface proteins in the past.
This raises the tantalising possibility that the reason some people experience more severe infections is that they haven’t got these hoards of T cells which can already recognise the virus. “I think it’s fair to say that the jury is still out,” says Hayday.
Unfortunately, no one has ever verified if people make T cells against any of the coronaviruses that give rise to the common cold. “To get funding to study this would have required a pretty Herculean effort,” says Hayday. Research into the common cold fell out of fashion in the 1980s, after the field stagnated and scientists began to move to other projects, such as studying HIV. Making progress since then has proved tricky, because the illness can be caused by any one of hundreds of viral strains – and many of them have the ability to evolve rapidly.
Will this lead to a vaccine?
If old exposures to cold viruses really are leading to milder cases of Covid-19, however, this bodes well for the development of a vaccine – since it’s proof that lingering T cells can provide significant protection, even years after they were made.
But even if this isn’t what’s happening, the involvement of T cells could still be beneficial – and the more we understand what’s going on, the better.
Hayday explains that the way vaccines are designed generally depends on the kind of immune response scientists are hoping to elicit. Some might trigger the production of antibodies – free-floating proteins which can bind to invading pathogens, and either neutralise them or tag them for another part of the immune system to deal with. Others might aim to get T cells involved, or perhaps provoke a response from other parts of the immune system.
“There really is an enormous spectrum of vaccine design,” says Hayday. He’s particularly encouraged by the fact that the virus is evidently highly visible to the immune system, even in those who are severely affected. “So if we can stop whatever it’s doing to the T cells of the patients we’ve had the privilege to work with, then we will be a lot further along in controlling the disease.”
It seems likely that we are going to be hearing a lot more about T cells in the future.
 |
July 21, 2020 — Study says actual number of Covid-19 cases is far greater than thought, CNN, (Commentary)
CNN reports that the number of people who have had Covid-19 is much greater than the official case count, according to data and a new analysis released by the US Centers for Disease Control and Prevention on Tuesday. Depending on the region and the time period, the number of people infected was anywhere between 2 and 24 times the number of reported cases, the CDC team said.
“For most sites, it is likely that greater than 10 times more … infections occurred than the number of reported Covid-19 cases,” the team wrote. In New York, the CDC estimates suggest that 642,000 people were infected by April 1 but at that point only 53,803 cases were officially reported. That means the number of infections could be at least 12 times higher than reported, the CDC said.
The CDC says the number of cases in South Florida, Connecticut and Minnesota was 6 to 11 times higher than the official count, the CDC said.
These numbers are likely conservative, according to the study in the Journal of the American Medical Association. The data used in the analysis was published on the CDC website.
The CDC has updated that data since the report was submitted to show two different testing periods starting in March and April. CDC Director Dr. Robert Redfield said last month that testing had likely missed 90% or so of cases. The country remains far from a level that would give the population herd immunity — assuming that having been infected once provides immunity. Doctors are not sure if that is the case.
Hours after the CDC analysis was released, President Donald Trump warned Americans that the pandemic will “probably, unfortunately, get worse before it gets better.”
Commentary — Sometimes good news comes in strange forms, and this is one of them.
This story is old news to anyone who has contacts in the medical field. The nurses I know have been saying for months that the official COVID-19 infection and death counts are way too low.
Now the CDC has officially concured with the nurses in the wards.
In New York City, for instance, the CDC now thinks the infection rate was 12 times greater than reported at the time. Stated another way, that means that the CDC missed more than 90 percent of the coronavirus cases this spring.
In New York City, this would mean there were 642,000 people infected by COVID-19 by April 1, not the paltry 53,803 infections that were officially reported at the time.
So how is this good news, you ask? It’s fabulous, dance-in-the-streets good news because it means that many, many more people than originally thought will now been exposed to COVID-19, and thrown it off, many of them without even knowing they were sick!
Not only have these heros of the pandemic demonstrated innate, inheritted strength against the disease, they now have some form of devloped immunity against COVID-19. We’re not sure exactly what yet, — but it will likely be expressed in the form of antibodies, T-cells, and possibly “immunological dark matter,” and it will convey SOME kind of increased immunity to COVID-19 because the people who threw off COVID-19 sight-unseen have now seen it before.
And this is EXACTLY what we’ve got to do to beat this pandemic — we’ve got to get the population to the herd immunity point, where enough people are immune that the disease can’t flare to wildfire proportions. This is how humanity has beatten every plague that’s ever challenged it, and it’s how humanity will beat this plague too, with or without a vaccine.
One true ray of good news on the coronavirus pandemic front right now are reports indicating that the hardest hit neighborhood in NYC have attained herd immunity, with more than 60 percent of the population tested showing antibodies to COVID-19, according to the New York Times.
A recent article in the Atlantic noted of New York:
Essentially, at present, New York City — which was hit very hard by the first coronavirus wave — might be said to be at a version of herd immunity, or at least safe equilibrium. Our case counts are very low. They have been low for weeks. Our antibody counts mean that a not-insignificant number of people are effectively removed from the chain of transmission.
However, the very idea of herd immunity is pretty upsetting for CNN, which ran an OpEd piece as a purported news story two weeks ago under the looney toones headline: “We’re wasting time talking about herd immunity” — never mind that herd immunity is the only path out available to us right now!
So this CNN COVID-19 story quickly and blandly looks past the good herd immunity news from New York, and reassures the reader that:
The country remains far from a level that would give the population herd immunity — assuming that having been infected once provides immunity. Doctors are not sure if that is the case.
Wheh! What a relief.
 |
July 23, 2020 – Bill Gates CBSN interview at-a-glance: Bill Gates on Coronavaccine Trials; Vaccine Side Effects, CBS
- Bill Gates warns you will probably need multiple doses of any given COVID-19 vaccine for it to be effective
- The Moderna COVID-19 vaccine (currently known only as mRNA-1273), caused systemic side effects in 80% of Phase 1 participants receiving the 100 microgram (mcg) dose
- Side effects ranged from fatigue (80%), chills (80%), headache (60%) and myalgia or muscle pain (53%). After the second dose, 100% of participants in the 100-mcg group experienced side effects
- In the 250-mcg dose group, 100% of participants suffered side effects after both the first and second doses. Three of the 14 participants (21%) in the 250-mcg group suffered “one or more severe events”
- According to Gates, the side effects are largely due to the high dosages Moderna had to use to achieve the desired antibody levels.
Commentary — Here’s the New England Journal of Medicine piece that provided the research backdrop for this interview.
 |
July 28, 2020 — How to Hold Beijing Accountable for the Coronavirus, Wall Street Journal
The closest known relative to SARS-CoV-2 is a virus sampled by Chinese researchers from six miners infected while working in a bat-infested cave in southern China in 2012. These miners developed symptoms we now associate with Covid-19. Half of them died. These viral samples were then taken to the Wuhan Institute of Virology—the only facility in China that’s a biosafety Level 4 laboratory, the highest possible safety designation. The Level 4 designation is reserved for facilities dealing with the most dangerous pathogens. Wuhan is more than 1,000 miles north of Yunnan province, where the cave is located.
If the virus jumped to humans through a series of human-animal encounters in the wild or in wet markets, as Beijing has claimed, we would likely have seen evidence of people being infected elsewhere in China before the Wuhan outbreak. We have not.
The alternative explanation, a lab escape, is far more plausible. We know the Wuhan Institute of Virology was using controversial “gain of function” techniques to make viruses more virulent for research purposes. A confidential 2018 State Department cable released this month highlighting the lab’s alarming safety record should heighten our concern.
Suggesting that an outbreak of a deadly bat coronavirus coincidentally occurred near the only level 4 virology institute in all of China—which happened to be studying the closest known relative of that exact virus—strains credulity…
Opinion By Jamie Metzl
 |
July 24 2020 — Pets show antibodies to SARS-CoV-2 in Italian study, Medical Life Sciences News
The current COVID-19 pandemic is caused by the SARS-CoV-2 coronavirus, which is thought to have originated in animals. This jumped species barriers to infect humans and is now showing rapid and easy transmission between them.
Medical Life Sciences News reports that a new study* shows that reverse transmission is probable, with 3-4% of a large number of domestic pets showing antibodies to the infection, though no virus was recovered from any animal.
Almost from the beginning, there have been reports that the virus can infect pet cats and dogs, with some animals showing symptoms of infection. Though these fears were initially decried, sporadic cases continue to be reported.
In these pets, the respiratory or fecal specimens, or both, have tested positive for the virus by reverse transcriptase polymerase chain testing (RT-PCR). Specific antibodies against the virus have also been detected in pet sera.
Targeted experiments also show that dogs are not easily infected and mostly develop an asymptomatic infection, with low viral titers being shed. On the other hand, cats show respiratory infection and shed high titers of the virus, and spread it to other animals as well.
The study: testing pets for SARS-CoV-2
The current study aimed at a more wide-scale testing of animal infection in their natural farm or home conditions. The researchers carried out a comprehensive survey of dogs and cats in Italy, from March to May 2020, in families with cases of COVID-19 or families living in severely affected areas.
Their own vets tested all the animals in the study during routine visits, including over 900 dogs and over 500 cats.
The samples were from nasopharyngeal, oropharyngeal or other severely affected areas in humans, or from other convenient sites. This yielded approximately 300 and 180 oropharyngeal swabs, 180 and 80 nasal samples, and 55 and 30 rectal swabs from dogs and cats, respectively.
Altogether, there were 1420 swabs, including around 40 dogs and cats each that were symptomatic at the time of sampling, and about 60 dogs and cats each from families that had one or more positive cases.
However, all were negative on PCR, including those living in households with confirmed cases of COVID-19 and those with and without respiratory symptoms. This suggests the animals were not actively infected at that time…
Implications and importance
The researchers point out, “This is the largest study to investigate SARS-CoV-2 in companion animals to date. We found that companion animals living in areas of high human infection can become infected.”
As often seen in humans, none of the animals below one year of age developed infection as assessed by PCR. This agrees with earlier research findings, and also indicates that older animals should be used in experimental studies, since otherwise the true susceptibility of the animal model may not be detected.
All animals tested positive by PCR, despite the significant percentage of seroconversion. This may mean that viral shedding is very short-lived in pet animals.
This has been observed in studies showing that shedding in cats ceases by 10 days following experimental infection, and neutralizing antibodies are detected by 13 days. In dogs, fecal samples showed the presence of the virus at up to 6 days post infection, but oropharyngeal swabs were negative.
The study notes that a natural infection in a Pomeranian, among the earliest reported, was associated with positive viral RNA in nasal swabs for 13 days, albeit at low levels, but not in fecal or rectal specimens. This may indicate variation in shedding pattern between animals.
Moreover, in another experimental animal study, half the dogs who were infected had demonstrable antibodies by 14 days. This indicates the difficulty in SARS-CoV-2 detection whether in humans or animals.
In the current study, the period that elapsed from infection to seroconversion is unknown. Even if the time of sampling was known, there could well have been delays in sampling due to the difficulty of visiting the vet during the period of lockdown. Therefore, the researchers advise that pets also be sampled to understand the true incidence of infection and viral shedding in the household and the community.
The researchers say that pets are unlikely to be an important route of viral spread, but when animals are present at high density, as on mink breeding farms, the virus may spread from animals to humans more readily.
Once the human-to-human spread is terminated, contact tracing will become more important. At that point, serologic surveys of pets may help provide a broad picture of the changing disease conditions within the community and an early warning of any transmission route left open.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
 |
July 27, 2020 — Two American coronavirus vaccines from Moderna and Pfizer begin the last phase of testing: 30,000-person trials, Washington Post, (Commentary)
The Washington Post reports that at 6:45 a.m. Monday, a volunteer in Savannah, Ga., received a shot in the arm and became the first participant in a massive human experiment that will test the effectiveness of an experimental coronavirus vaccine candidate. The vaccine is being developed by the biotechnology company Moderna in collaboration with the National Institutes of Health.
The vaccination marks a much-anticipated milestone: the official launch of the first in a series of large U.S. clinical trials that will each test experimental vaccines in 30,000 participants, half receiving the shot and half receiving a placebo. Pharmaceutical giant Pfizer also announced it was initiating a 30,000-person vaccine trial, at 120 sites globally.
“We are participating today in the launching of a truly historic event in the history of vaccinology,” Anthony S. Fauci, director of the National Institute of Allergy and Infectious Diseases, said at a news conference. He noted that the United States has never moved faster to develop a vaccine, from basic science to a large Phase 3 trial designed to test safety and effectiveness.
Fauci predicted that researchers would probably be able to tell whether the Moderna vaccine was effective by November or December, although he explained that it was a “distinct possibility” an answer could come sooner. Pfizer officials have said the company expects to be able to seek regulatory authorization or approval by October.
Company and government officials repeatedly underscored that although the vaccine development effort is moving at record-breaking speed, safety is not being sacrificed.
“There is no compromise at all, with regard to safety, nor of scientific integrity,” Fauci said.
Both vaccines require two doses, spaced several weeks apart. Then researchers will have to wait to see whether people get infected or sick from the novel coronavirus. What they hope to witness is a clear benefit: fewer infections in people who received the vaccine, or less severe episodes of covid-19, the disease caused by the coronavirus. There are many unknowns about how long it could take to see a clear signal of success or failure — including how fast the trials will recruit participants and how long it takes for enough people to become infected to observe whether there is an effect.
Statisticians have been crunching the numbers to predict how many infections would need to occur in the study population to gauge the vaccine’s effectiveness. To show the Moderna vaccine is 60 percent effective, Fauci said, there would need to be about 150 infections among the 30,000 participants.
The trials are also the biggest test yet of a promising technology that has never been approved for use outside medical research. Either vaccine could become the first in a new class of medicines. The vaccines deliver a snip of genetic material that carries the blueprint for the spiky protein that dots the surface of the coronavirus. After a person is vaccinated, their cells will follow the genetic instructions to build the proteins, and their immune systems, confronted with the spike protein, learn how to recognize and mount a defense to the virus without ever being infected.
Commentary — wow, it’s really exciting to see how excited everyone is about this exciting news, and all the exciting experimental whiz bang medical technology that’s gone into the exciting press release, er, story in the Post by Carolyn Y. Johnson!
Since the Russians completed human trials on a COVID-19 vaccine nearly a month ago, it’s interestingly, that the Post story makes no mention of the Russian vaccine candidates, even though the race for a coronavirus vaccine is the biggest American / Russian technology faceoff since Sputnik!
And speaking of Sputnik, 1957 (the year the Soviets lauched Sputnik 1 into orbit around the earth), was also the year that another deadly viral pandemic swept out of China, namely the Asian flu pandemic.
Like COVID-19, the Asian flu was another novel coronavirus that may have crossed the species lines to become infective to humans. The Asian flu had a mortality rate very similar to COVID-19 and killed nearly 120,000 Americans in 1957-58, a far larger percentage of the total American poplation than COVID-19 has killed so far in 2020.
The big difference between the Asian flu in 1957 and the coronavirus in 2020 is that the United States was able to develop and distribute an effective vaccine within six months of the first international outbreak of the Asian flu in Singapore and Hong Kong.
So if the American immuneological experts were as sharp today as the Russians, of even as good as the Americans were nearly 60 years ago, they’d have delivered an effective vaccine and begun distribution LAST MONTH!
And what was Carolyn Y. Johnson thinking when she wrote in her best talking head video news on the scene prose:
Company and government officials repeatedly underscored that although the vaccine development effort is moving at record-breaking speed, safety is not being sacrificed.
“[R]ecord breaking speed”? Only if you ignore what the Russians did a couple weeks ago and what America could do in 1957.
Still, I have to say — Carolyn Y. Johnson is such an exciting young talent!!!
 |
July 29, 2020 – Old Vaccines May Stop the Coronavirus, Study Hints. Scientists Are Skeptical, New York Times
The New York Times reports that billions of dollars are being invested in the development of vaccines against the coronavirus. Until one arrives, many scientists have turned to tried-and-true vaccines to see whether they may confer broad protection, and may reduce the risk of coronavirus infection, as well.
Old standbys like the Bacille Calmette-Guerin tuberculosis vaccine and the polio vaccine appear to help train the immune system to respond to a broad variety of infections, including from bacteria, viruses and parasites, experts say.
Now a study suggests that people who have received certain routine vaccines in the recent past — including childhood vaccinations like measles-mumps-rubella and polio, as well as adult flu vaccines — have lower coronavirus infection rates than those not recently vaccinated.
But many experts greeted the conclusions with skepticism. The paper, an analysis of electronic health records from the Mayo Clinic, was posted online; it has not been through the peer review process and has not been accepted by a medical journal.
Critics pointed to numerous methodological problems. It is a retrospective study; as such, it points to an association between vaccinations — a marker of overall good health and healthy behaviors — and lower infection risk.
But the study does not prove a cause-and-effect relationship. While scientists generally consider studies like these useful for generating hypotheses that may be worth exploring further, they are far from definitive.
The researchers analyzed the immunization records of 137,037 patients who had been tested for infection with the coronavirus, comparing matched pairs of vaccinated and unvaccinated patients who were otherwise similar.
Patients had lower infection rates if they had recently been given the high-dose flu vaccine or had been vaccinated against polio, measles-mumps-rubella, chickenpox, pneumococcal disease, hepatitis A and hepatitis B, or haemophilus influenzae Type B, compared with those who had not received those vaccines in recent years.
The level of risk reduction varied, depending on the vaccine and on how recently the individual had been vaccinated. But generally, the childhood vaccinations were linked to a greater reduction in coronavirus infection than the high-dose flu vaccine given to elderly individuals.
And some vaccines, if received five years before the study began, were tied to higher coronavirus infection rates, including the human papillomavirus vaccine and the one against typhoid, as well as the meningococcal vaccine.
The researchers went to great pains to account for variables that might have made a difference, including testing rates and geographic variations in coronavirus rates, as well as demographic factors like age, race and ethnicity, though some critics said these efforts fell short.
“The hypothesis we are testing is that the immune system memory is stimulated by the vaccine,” said one of the authors of the paper, Venky Soundararajan, the founder of nference, a company that uses artificial intelligence to synthesize biomedical information.
“Then along comes SARS-CoV-2,” he said, “and the immune system is able to get the virus to back off and to clear it, so it can’t invade multiple cells and become a full-blown infection.”
In one dramatic finding, Black patients who had received the pneumococcal disease vaccine five years before the study had a significantly lower risk of testing positive for the coronavirus, compared with similar patients who had not gotten the vaccine. That vaccine protects against 13 types of bacteria, including some that cause pneumonia.
But experts said the findings should be interpreted with great caution.
“Retrospective studies are great and they provide some hints, but there are caveats,” said Dr. Shyam Kottilil, a professor of medicine with the Institute of Human Virology at the University of Maryland School of Medicine. “It’s very difficult to establish causality.”
 |
July 31, 2020 — Dozens of COVID-19 vaccines are in development. Here are the ones to follow, National Geographic (Commentary)
Name: mRNA-1273
Who: A Massachusetts-based biotech company, in collaboration with the National Institutes of Health.
What: This vaccine candidate relies on injecting snippets of a virus’s genetic material, in this case mRNA, into human cells. They create viral proteins that mimic the coronavirus, training the immune system to recognize its presence. This technology has never been licensed for any disease. If successful, it would be the first mRNA vaccine approved for human use. (Here’s how mRNA vaccines work.)
Status: On July 27, Moderna announced it had started the third phase of its clinical trials, even as it continues to monitor phase two results. Preliminary findings from phase one have shown that healthy subjects produced coronavirus antibodies and a reaction from T-cells, another arm of the human immune response. Phase three will test the vaccine in 30,000 U.S. participants. Moderna says it is on track to deliver at least 500 million doses per year beginning in 2021, thanks in part to the deal it has struck with Swiss manufacturer Lonza that will allow it to manufacture up to one billion doses a year.
Name: BNT162b2
Who: One of the world’s largest pharmaceutical companies, based in New York, in collaboration with German biotech company BioNTech.
What: Pfizer and BioNTech are also developing an mRNA vaccine based on the German company’s earlier efforts to use the technology in experimental cancer vaccines. Pfizer has signed a nearly $2 billion contract with the U.S. government to provide 100 million doses by December 2020—an agreement that goes into effect when and if the drug is approved and delivered.
Status: On July 27, Pfizer and BioNTech launched a trial that combines phase two and three by enrolling a diverse population in areas with significant SARS-CoV-2 transmission. It will examine the vaccine’s effect in 30,000 people from 39 U.S. states and from Brazil, Argentina, and Germany. The project is aiming to seek regulatory review as early as October 2020 to meet the December deadline—and hopes to supply 1.3 billion doses by the end of 2021. Preliminary results of phase one/two data show the vaccine produces antibodies and T-cell responses specific to the SARS-CoV-2 protein.
Name: ChAdOx1 nCoV-19
Who: The U.K. university, in collaboration with the biopharmaceutical company AstraZeneca.
What: Oxford’s candidate is what’s known as a viral vector vaccine, essentially a “Trojan horse” presented to the immune system. Oxford’s research team has transferred the SARS-CoV-2 spike protein—which helps the coronavirus invade cells—into a weakened version of an adenovirus, which typically causes the common cold. When this adenovirus is injected into humans, the hope is that the spike protein will trigger an immune response. AstraZeneca and Oxford plan to produce a billion doses of vaccine that they’ve agreed to sell at cost.
Status: Preliminary results from this candidate’s first two clinical trial phases revealed that the vaccine had triggered a strong immune response—including increased antibodies and responses from T-cells—with only minor side effects such as fatigue and headache. It has now moved into phase three of clinical trials, aiming to recruit up to 50,000 volunteers in Brazil, the United Kingdom, the United States, and South Africa.
Name: CoronaVac
Who: A Chinese biopharmaceutical company, in collaboration with Brazilian research center Butantan.
What: CoronaVac is an inactivated vaccine, meaning it uses a non-infectious version of the coronavirus. While inactivated pathogens can no longer produce disease, they can still provoke an immune response, such as with the annual influenza vaccine.
Status: On July 3, Brazil’s regulatory agency granted this vaccine candidate approval to move ahead to phase three, as it continues to monitor the results of the phase two clinical trials. Sinovac says the first phases have so far shown that the vaccine does produce an immune response with no severe adverse effects. Preliminary results of this candidate’s earlier testing in macaque monkeys, published in Science, revealed that the vaccine produced antibodies that neutralized 10 strains of SARS-CoV-2. Phase three will recruit nearly 9,000 healthcare professionals in Brazil.
Name: None
Who: China’s state-run pharmaceutical company, in collaboration with the Wuhan Institute of Biological Products.
What: Sinopharm is also using an inactivated SARS-CoV-2 vaccine that it hopes will reach the public by the end of 2020. Sinopharm has reported that early trials of its vaccine candidate triggered a strong neutralizing antibody response in participants, with no serious adverse effects.
Status: In mid-July, Sinopharm launched its phase three trial among 15,000 volunteers—aged 18 to 60, with no serious underlying conditions—in the United Arab Emirates. The company selected the UAE, as it has a diverse population with approximately 200 different nationalities, making it an ideal testing ground.
Murdoch Children’s Research Institute
Name: Bacillus Calmette-Guerin BRACE trial
Who: The largest child health research institute in Australia, in collaboration with the University of Melbourne.
What: For nearly a hundred years, the Bacillus Calmette-Guerin (BCG) vaccine has been used to prevent tuberculosis by exposing patients to a small dose of live bacteria. Evidence has emerged over the years that this vaccine may boost the immune system and help the body fight off other diseases as well. Researchers are investigating whether these benefits may also extend to SARS-CoV-2, and this trial has reached phase three in Australia. Though as of April 12, the World Health Organization says there is no evidence that the BCG vaccine protects people against infection with the coronavirus.
Status: In April, researchers from the Murdoch Children’s Research Institute began a series of randomized controlled trials that will test whether BCG might work on the coronavirus as well. They aim to recruit 10,000 healthcare workers in the study.
Name: Ad5-nCoV
Who: A Chinese biopharmaceutical company.
What: CanSino has also developed a viral vector vaccine, using a weakened version of the adenovirus as a vehicle for introducing the SARS-CoV-2 spike protein to the body. Preliminary results from phase two trials, published in The Lancet, have shown that the vaccine produces “significant immune responses in the majority of recipients after a single immunisation.” There were no serious adverse reactions documented.
Status: Though the company is still technically in phase two of its trial, on June 25, CanSino became the first company to receive limited approval to use its vaccine in people. The Chinese government has approved the vaccine for military use only, for a period of one year.
HERE’S A sweet little “false news” piece that keeps lurching to one side like a car with a front tire that’s going flat, and finally ends up in the ditch after what looked like a tremendously promising start.
Actually, the best thing about the start is what happened before the start. A+ to whoever at National Geographic was responsible for the original story concept and shaping. It’s slick, intriguing, smartly timely and professional and everything it should be.
The design and illustration are likewise excellent, and I found myself idly staring at the lead illustration featuring a photo by Hans Pennick that I would call a nearly “perfect” pop magazine illustration for August 2020 in America.
Pennick’s photo captures COVID-19 volunteer Melissa Harting, of Harpersville, NY, a 30ish woman with blue hair and lots of accessorized blue tattoos, as she archly considers the flu shot she is about to receive.
THEN, HOWEVER, comes the story itself.
Speaking personally, I’ve never really gotten terribly heated up about “false news” because, as an ex-wife of mine (who was a lawyer turned mediator) once said to me, “there are ALWAYS two sides to a story, and frequently more!”
And as a journalist with 50 years professional experience from the trenches to the towers, my personal experience tells me: nobody owns the truth. The truth serves no one party, cause, nation, religion, race or hair style.
That said, there is this gaping, naked right there in public in front of all those people “false news” interlude near the beginning of Amy McKeever’s story where McKeever, her fact checkers and editors simply let a big bald self-congratulatory falsehood slip through, and then used it to support further falsehood.
The matter at issue is McKeever’s assertion that:
It can typically take 10 to 15 years to bring a vaccine to market; the fastest-ever—the vaccine for mumps—required four years in the 1960s.
Unfortunately, that’s just not true. Thanks to Maurice Hilleman, chief of respiratory diseases at the Walter Reed Army Institute of Research in Washington, D.C., in 1957, the United States was able to develop and distribute an effective Asian flu vaccine within six months of the first international outbreak of the Asian flu in Singapore and Hong Kong.
So the fastest vaccine on record is actually the Asian flu, which took six months in 1957, not the mumps, which took four years “in the 1960s,” as McKeever has it.
Over-looking this inconvenient detail, McKeever then uses the false assertion that the mumps was the fastest vaccine ever developed to suggest that the coronavirus vaccine contestants today are chasing a vaccine development world speed record — and even praises their plucky effort “to bring one to market in record time” — when in fact the mumps vaccine was not the fastest, and the chance to break the vaccine development speed record already passed last month.
OK, SO everybody makes mistakes. Let me tell you I have made my share of ’em, and Amy McKeever won’t be the last either.
So I shrugged and read on in the National Geographic‘s rundown on coronavirus vaccine contestants. First up was Moderna Theraputics (mRNA-1273), an experimental mRNA vaccine.
Amy McKeever is pretty upbeat about this Big Pharma vaccine contestant. She likes their experimental whiz-bang genetic engineering technology and their positioning in the process, and she makes no mention at all about side affects reported for Moderna’s mRNA-1273 coronavirus vaccine candidate.
And she ESPECIALLY doesn’t mention the recently published article in the New England Journal of Medicine stating that in the highest mRNA-1273 dosage group, which received 250 mcg, 100% of participants suffered side effects after both the first and second doses. In addition, three of the 14 participants (21%) in the 250-mcg group suffered “one or more severe events.”
Bill Gates was even interviewed by CBS-TV on July 23 about the side effects problems with Moderna’s mRNA-1273 coronavirus vaccine candidate, so none of the side effect information that Amy McKeever and National Geographic missed was exactly hiding.
Was this another right-out-in-plain-sight screwup? It’s McKeever’s job to know about the New England Journal of Medicine study on Moderna’s mRNA-1273 vaccine side effects before the article appears. Did she fail to do her job? Well maybe, but it’s also very possible that the National Geographic (which probably has the longer production schedule) was already locked in on the final form of McKeever’s article before she got wind of the New England Journal of Medicine study.
So I kept reading, and I must admit I enjoyed the article on balance, and I learned a couple things from it.
But after I finished it and figuratively threw it down on the table, something was bothering me. I couldn’t figure out what it was immediately, but later it came to me.
This story has a gaping hole in the center because it is missing all mention of the most important player on the entire coronavirus vaccine landscape. That would be the Russians, who were the first to complete human trials, and have announced widespread introduction of the new vaccine by October 2020, months before anyone else.
Somehow, knowledge of these well-publicized Russian COVID-19 vaccine advances were kept from Amy McKeever by occult means? Perhaps the same occult wavelength that prevented her knowing about Moderna’s side effect issues?
MY VIEW? Even though there are some plausible excuses for each of the three big mistakes in this article, the three gotchas here (getting the fastest vaccine development wrong, omitting the side effects reports on Moderna’s vaccine candidate, and ignoring the Russians, who are the leader and therefore biggest player in the whole vaccine story) make this National Geographic story by Amy McKeever one of the least competent national magazine pieces I can remember. This thing is a real “cluster fuck,” as the Vietnam vets say.
And where were the editors?
 |
July 31, 2020 — China’s coronavirus vaccines face hurdles, Nature
Nature writes that Chinese companies are at the forefront of global efforts to create a vaccine for the coronavirus, with more than half a dozen candidates in clinical development. Last week, Tianjin-based CanSino Biologics published results1 from an early-stage clinical trial showing that its vaccine is safe and can trigger an immune response.
Yet the companies could face difficulty as they try to push vaccines through phase III trials, a crucial stage of testing that is needed to prove efficacy and secure approval from regulators. These trials usually require tens of thousands of participants, and with the outbreak in China largely under control, companies are having to test their vaccines elsewhere. But researchers say they might still struggle to enrol so many participants and employ enough health-care professionals to collect data.
“The Chinese companies will need to step outside of China,” says Jerome Kim, director-general of the International Vaccine Institute in Seoul. “The race is on,” he says, “and it’s really about who can set up in a high-risk area most quickly.”
Chinese vaccine-makers will face other challenges, too. Vaccines will probably face extra scrutiny, given the country’s opaque regulatory system and previous vaccine scandals, say scientists. In 2018, hundreds of thousands of children reportedly received defective diptheria, tetanus and whooping cough vaccines.
Quick to act
As the country where the coronavirus outbreak began, China was fast out of the gate in developing vaccines. CanSino’s offering is made from a common-cold virus, tweaked to mimic the coronavirus. Sinopharm, a state-owned pharmaceutical company in Beijing, is developing two vaccines made using particles of the coronavirus that have been inactivated so that they can no longer cause disease. The company said in press releases in June that both vaccines had produced antibodies in all participants in preliminary phase I and II trials. And Beijing-based company Sinovac has announced similarly promising results for its own inactivated-virus vaccine.
This month, Sinovac launched a phase III trial of its vaccine in Brazil. Sinopharm will be testing its inactivated vaccines in the United Arab Emirates (UAE). Only three other coronavirus vaccines have entered phase III trials: one produced by biotech company Moderna in Cambridge, Massachusetts; one by the University of Oxford and drug maker AstraZeneca, based in Cambridge, UK; and one by biotech company BioNTech of Mainz, Germany, in collaboration with New York City-based drug firm Pfizer.
CanSino is also poised to launch a phase III trial. But the Chinese government has already said that its vaccine can be used by the military — making CanSino the first company to have a vaccine for COVID-19 approved for limited use in people. China has worked hard “to generate an efficient vaccine as soon as possible and to be transparent” when doing so, says Stéphane Paul, a vaccine researcher at the University of Lyon in France.
The speed with which Chinese vaccine-makers are moving has raised hopes around the world. Sinopharm has even promised to have a vaccine ready to distribute by the end of the year.
Inactivated vaccines are widely used vaccine types, so it makes sense for Chinese companies to focus on them, says Paul. “As a first line of vaccine, it is immunogenic, quick to develop and low-cost,” he says.
But some viruses become more potent when they infect organisms previously treated with inactivated vaccines, in a poorly understood phenomenon known as antibody-dependent enhancement (ADE). This was reported2 last year in monkeys given a vaccine for the coronavirus that causes severe acute respiratory syndrome (SARS). Sinovac says its COVID-19 vaccine did not trigger ADE in monkeys, but the risk will be closely monitored in all the inactivated-vaccine phase III trials, says Paul.
Hurdles ahead
Some observers also question whether companies will be able to work at the promised speed, and with the precision that such trials require. And the fact that China was willing to approve CanSino’s vaccine for use in the military before phase III trials were complete raised eyebrows. “The decision is political, and not scientific in nature. It doesn’t demonstrate anything on the potential efficacy of this vaccine,” says Marie-Paule Kieny, a vaccine researcher at INSERM, the French national health-research institute, in Paris.
Phase III trials present challenges for vaccine-makers around the world, such as the need to recruit enough participants and qualified health staff. Demonstrating that vaccines provoke an immune response and protect people from the virus requires data on 20,000–40,000 people who have been split into control and test groups and then followed closely for several months or even years, scientists say. To reach the numbers required, the trials might need to combine results from dozens of hospitals, each supplying data from hundreds of patients. “All of these things have to be done, and done correctly,” says Kim. “The number of sites that can do this and handle the volume is limited,” he adds. “Even the best sites will have difficulty.”
Many Chinese companies are at a disadvantage because they don’t have established networks of hospitals around the globe, says Kim. AstraZeneca, which published3 promising early trial results for its vaccine — based on a chimpanzee cold virus — the same day as CanSino, is carrying out phase III studies in the United Kingdom, Brazil and South Africa. Moderna has launched a trial of its vaccine, which elicits an immune response with synthesized RNA that mimics the RNA that the coronavirus uses to replicate, in 30,000 people across the United States, a country with a lot of experienced clinical researchers to carry out trials, and a large coronavirus outbreak.
US President Donald Trump said last week that he was willing to work with any country that can deliver an effective vaccine, but Chinese companies had previously been ruled out of receiving funding from the US government’s Operation Warp Speed, which aims to speed vaccine development. The possibility of a US–China collaboration was also damaged on 21 July, when the US Department of Justice made public allegations that two Chinese hackers had tried to steal COVID-19 vaccine designs from a US company.
Still, Kieny points out that Sinopharm has partnered with the UAE’s government and Group 42 Healthcare, a local artificial-intelligence company, for its phase III trial, and Sinovac has partnered with the Butantan Institute in São Paulo, Brazil. “So far, Chinese companies seems to have been successful in finding partners,” she says.
Sufficient data?
But some researchers question whether the trials in the UAE and Brazil will gather enough data to convince regulatory agencies that the vaccines work. In the UAE, where Sinopharm plans to enrol 15,000 participants to study its two vaccines, relatively few people are infected with COVID-19.
And although Brazil has a large coronavirus outbreak, the Butantan Institute plans to test Sinovac’s vaccine among health-care professionals because it is assumed they will face greater exposure to the virus than will non-health-care professional. Because of this, the trial will enrol only 9,000 people to test whether it works, says Ricardo Palacios, a clinical researcher at the institute who is leading the trial. “We designed a trial in order to obtain answers in a more efficient way,” says Palacios.
Kim notes that in countries where health-care workers wear proper personal protective equipment, they might not face greater exposure to the virus, which would undermine the justification for a smaller trial.
The most important thing is that trials collect data that adhere to international standards expected by drug regulators and by bodies such as the World Health Organization, says Kim. “If you can’t do that, you’re in trouble,” he says.
 |
August 1, 2020 — Russia plans mass vaccinations by October, doctors and teachers will be first, health officials said, Fox News
Fox News reports that Russian health officials say a potential coronavirus vaccine that finished clinical trials in Moscow two weeks ago (the first and so-far only COVID-19 vaccaine candidate in the world to get over this necessary hurdle), could be in mass production by October.
Health Minister Mikhail Murashko said the Russian state research facility Gamaleya Institute is one step closer to registering the vaccine, according to Interfax news agency.
Murashko said that upon approval, the vaccine would be available first to health care workers, then teachers.
Russia’s first potential vaccine would secure local regulatory approval in August, a source told Reuters.
But the fast pace of production of the adenovirus-based vaccine — coming just five months after COVID-19 became widespread in Russia — has given pause to Western experts, who question the adequacy of testing for the drug.
The vaccine is essentially a common cold virus fused with the spike protein of SARS CoV-2 to prompt an immune response.
Dr. Anthony Fauci, head rah-rah guy for Big Pharma in the U.S. who is sometimes described as a leading American infectious disease expert, sniffed that he hoped that Russia, China and other international competitors racing for a vaccine were “actually testing the vaccine” before administering them to anyone.
Commentary — Hey Tony, way to stand tall for the little guy. But you know, it took the U.S. just six months to develop a vaccine for another smiliarly deadly novel coronavirus, the Asian flu pandemic of 1957. Going by that proven American novel coronavirus vaccine timetable, the U.S. should have had a COVID-19 vaccine through human trials and in production by LAST MONTH!
 |
August 3, 2020 – Russia gears up for mass vaccination against coronavirus despite international skepticism, CNBC
CNBC reportes that Russia is preparing to start a mass vaccination campaign against the coronavirus in October.
Health Minister Mikhail Murashko said clinical trials of a coronavirus vaccine candidate from the Moscow-based Gamaleya Institute were complete, Russian state news agency RIA reported Saturday. Moscow has claimed the test results showed an immune response in all subjects, with no side effects or complications.
Russia has completed early-stage clinical tests with the vaccine candidate from the institute, a spokesman for Russia’s RDIF sovereign wealth fund told CNBC on Monday. The country is now set to begin large-scale phase three trials this month. This phase of clinical research is the only way to show whether a vaccine is effective.
According to the World Health Organization, there are 26 candidate vaccines in clinical trials around the world, including an early-stage one from the Gamaleya Institute. But the WHO has not listed any second or third-phase trials from the country and did not immediately respond to a CNBC request for comment on Russia’s vaccine claims.
The laboratory behind the vaccine is now seeking regulatory approval for the drug, Murashko said according to RIA, and that this would be required before it could be used. Doctors and teachers would be the first to be vaccinated, he said, while mass vaccinations are planned for October.
Industry and Trade Minister Denis Manturov told Russia’s TASS news agency Monday that the country was expecting to manufacture several million doses of Covid-19 vaccines each month by the start of 2021.
This acceleration of Russia’s vaccine development could mean the country will become the first in the world to inoculate people against the virus, a huge milestone in combating a pandemic that has claimed the lives of more than 689,000 people worldwide.
“It’s a Sputnik moment for many people who didn’t expect Russia to be the first,” RDIF CEO Kirill Dmitriev told Abu Dhabi newspaper The National last week. RDIF has been involved in funding the country’s vaccine research.
International skepticism
However, there has been much international skepticism surrounding Russia’s vaccination efforts. White House coronavirus advisor Dr. Anthony Fauci, for instance, has cast doubt on the approaches to testing in Russia and China.
“I do hope that the Chinese and the Russians are actually testing the vaccine before they are administering the vaccine to anyone,” Fauci said in a congressional hearing on the coronavirus crisis on Friday.
“I do not believe that there will be vaccines, so far ahead of us, that we will have to depend on other countries to get us vaccines.”
And Britain’s Telegraph newspaper reported Saturday that London would likely reject Russia’s Covid-19 vaccine due to doubts over the trial process. Russia has released no scientific data as to the safety and effectiveness of its vaccine.
Last month, Russia was accused by officials in the U.S., Canada and Britain of trying to hack and steal coronavirus vaccine data. China has also been accused by Washington of hacking into the computer systems of firms working on a Covid-19 vaccine.Moscow and Beijing have rejected the allegations, claiming they weren’t backed by evidence.
Russia has the fourth-highest number of coronavirus infection in the world, according to Johns Hopkins University data, with over 854,000 people having tested positive. More than 14,000 have died from Covid-19, while around 649,000 have recovered after contracting the disease.
Last month, an early-stage human trial of a vaccine candidate conducted by Oxford University and AstraZeneca indicated it was safe and produced a strong immune response, according to The Lancet medical journal.
There has also been promising data from vaccine candidates being developed by U.S. biotechnology company Moderna, as well as American drugmaker Pfizer and German biotech firm BioNTech.
Nearly 1.5 million people in Italy have coronavirus antibodies: study, Local IT, 8/4/2020 (Commentary)
Nearly 1.5 million people in Italy have probably developed coronavirus antibodies, according to a nationwide study, more than six times the number of people who tested positive for the new virus.
The Local IT writes that preliminary results from thousands of blood tests conducted across Italy in the past two months suggest that the number of people exposed to the coronavirus was far higher than the number of infections officially confirmed – 248,229 to date.
According to the Ministry of Health, 1.482 million people – the equivalent of 2.5 percent of the entire population of Italy – are believed to have coronavirus antibodies in their blood, which indicates that they have been exposed to the virus and had an immune response, but not whether they’re safe from catching it again.
The findings are based on nearly 65,000 blood tests on a cross-section of Italian residents, carried out between late May and mid July by the Italian Red Cross on behalf of the Health Ministry and national statistics office Istat.
More than a quarter of people found to have antibodies, 27.3 percent, never developed any symptoms of Covid-19, which the health ministry said emphasised the importance of following social distancing and hygiene rules to avoid spreading the virus unwittingly.
“The rate of 2.5 percent might seem low but it can become problematic if we’re not cautious,” said Gian Carlo Blangiardo, president of Istat, as the researchers presented their first results on Monday.
“It means that the probability of encountering someone positive for the virus is 2.5; if I encounter 20 people, there’s a 50 percent chance I’ll come into contact with someone positive.”
The rate was significantly higher in parts of northern Italy, where most of Italy’s coronavirus cases have been recorded.
In Lombardy, the northern region with the biggest number of infections by far, 7.5 percent of people tested had coronavirus antibodies – three times the national average. In the worst affected province of Bergamo, the rate was as high as 24 percent.
The highest regional rates were all in the north of Italy, while they were below the national average almost everywhere in the centre and especially the south. At the lowest end of the scale, the rate among residents of Sicily and Sardinia was just 0.3 percent.
Predictably, antibodies were more prevalent in health workers, 5.6 percent of whom showed signs of exposure. There was also an elevated rate among people working in restaurants, 4.1 percent…
The researchers carried out 64,660 blood tests between May 25th and July 15th. Participants came from a sample of 150,000 people across 2,000 municipalities and a range of ages and professions who were originally invited to take part. All of those selected lived with other members of their family, i.e. not alone, with housemates or in nursing homes.
Commentary — more good news for herd immunity!
 |
August 5, 2020 — Sweden’s top virologist has a message on how to defeat coronavirus: Open schools and no masks, Fortune
Fortune writes just a month ago, Sweden was labeled the “world’s cautionary tale” for its laissez-faire approach to fighting the coronavirus. It famously decided not to close its schools, restaurants or bars, and it told its citizens that there’s no need to mask-up. When the death toll surged in late April, and the country looked overmatched by the fast-moving virus, its officials sounded defensive.
The country’s Public Health Agency developed and implemented Sweden’s approach, and its chief epidemiologist, Anders Tegnell, became the face of the crisis.
While other countries were locking down shops, schools, and public life, Sweden was the outlier, trying to manage the disease with the least possible impact on the economy. The prominent Swedish virologist Lena Einhorn, for one, called the Sweden approach “madness.” Seeing the mortality rate climb in Sweden, Norway decided to close its border with its chief trading partner.
By a per-capita basis, the coronavirus outbreak in Sweden has been one of the world’s deadliest—worse than the United States, France, or any Nordic neighbor. But in the past six weeks, Sweden has seen a remarkable turnaround. New daily cases are down to multi-month lows. Hospital admissions are close to zero, and just 44 Swedes died of COVID-19 in the past seven days, official numbers show. At the same time, coronavirus cases are spiking around continental Europe.
Tegnell feels vindicated by the latest batch of promising data.
Last week, he told reporters that masks are not necessary in Sweden. In an interview with Fortune this week, he doubled down on that message, saying the sustained flattening of the curve tells him to not change a thing about the country’s mask strategy—or anything else for that matter.
“We don’t have to introduce masks right now. Because, with a down-going trend,” he said, “it’s not the time to introduce new measures.”
Better than nothing
The mask debate is dividing lawmakers and scientists alike, even as a wave of new studies show that some kind of mouth-and-nose covering is better than nothing in protecting against infection and/or spreading the virus to someone else in the vicinity.
Tegnell has reviewed the body of research and isn’t convinced the mask is an effective tool in a public health threat like the coronavirus. The flaw in the mask strategy comes down to you and me, he says.
“The mask,” he allows, “is complicated. You have to decide when to use them, who should use them, and then try to find out if will you be able to use them properly in a context. I mean, we’re talking about masks in restaurants, and, of course, you cannot eat with a mask on.” And, he pointed to Spain, which has a relatively strict mask rule but where cases have spiked lately.
He adds: “I’m telling people it’s much better to keep a social distance. This is really the best thing you can do in trying to lessen the risk of [infection]—keeping distance. Try to work from home, cycle to work instead of taking the bus if you can. There are plenty of things you should do before you start with a mask [policy].”
Never mind that in, say, the New York metropolitan area, which has a population double that of the whole of Sweden, it’s not easy to maintain social sufficient social distancing. On either side of the Hudson, the Sweden model—as it pertains to masks, at least—won’t be all that applicable.
Stay in school
Tegnell believes Sweden could serve as a model on another thorny issue: schools.
In the spring, Sweden opted not to close its daycare centers or schools, and, Tegnell contends, it had little bearing on infection rates. The Public Health Agency compiled the data on its schools-policy decision and shared its results. Sweden reported 1,124 cases of school-aged children contracting COVID-19 in a period spanning from March, when the outbreak began, to the close of the school year in mid-June. That number equals 2.1% of all COVID cases in the country during that period. Of those, 14 had to be hospitalized in an intensive care unit.
Sweden contrasts those numbers with those of Finland.
“Finland kept the schools closed, and we kept them open. And it seems like, at least in our context, it didn’t make a huge difference, neither to the pandemic, nor to the number of children falling ill,” Tegnell told Fortune.
“It seems like children do get infected,” he continued. “They very seldomly get seriously ill, and they don’t seem to spread the infection very much to other parts of the society.”
The comparative data bears this out. Partly. Even though they were at home much of the final three months of the school year, Finnish school-aged children, on a per-capita basis, caught the coronavirus at a rate that was nearly four times higher than their counterparts in Sweden. But just one Finnish child was admitted to the ICU compared to 14 in Sweden.
As most parents would tell you, just 14 kids in the ICU is hardly reassuring data.
Still, Tegnell believes school kids are low-risk virus vectors who ought to be in classrooms, not at home distance-learning. “Keeping schools open is quite possible to do without having any negative effects,” he said.
Medical professionals elsewhere are not so sure. Researchers in the United States last week, for example, found that COVID-infected children under five were major carriers of the virus.
Flowers and cards
Tegnell mentioned more than once the “ethics” of Sweden’s public health policy. For example, the public health experts decided early on that a policy of achieving herd immunity, as was discussed in Great Britain, was out of the question in Sweden. “Of course, we will not let people fall ill just to achieve herd immunity. That’s not the way we’re working,” he said. Besides, he later said, sufficient herd immunity is neither achievable nor would it be sustainable with coronavirus.
And yet the “Swedish model” has become synonymous with a leave-the-people-alone approach to managing a public health crisis, a strategy advocated by small government advocates around the world. This puzzles Tegnell. The objective in Sweden was the same as everywhere else, he says: to get the infection numbers down.
“When I talk with my colleagues in the UK, for example, we could see that we were able to achieve in Sweden almost the same kind of things that they were able to achieve by legal measures—that is, to encourage people to maintain social distance and so on,” he said.
How Sweden achieved this wasn’t through a strict set of rules, it was by winning the people over. “We have a very high level of trust among the population,” he said.
Each week, the health agency collects survey data from thousands of Swedes. In it, they asked a big question: How are we doing? The approval rate has been sky high.
“It seems 80% of the people, when asked, ‘Are you following the advice of the agency?’ responded, ‘Yes, we are following the advice of the agency.’ And that’s been consistent all the way through,” he said. “The trust for the agency is high. People continue to follow our advice. I think that’s really important.”
“It’s rather unusual that an agency in Sweden gets flowers from the population—flowers and cards.”
Commentary — Amazing, in all the world and all the people in the world, there turned out to be one nation, and one man, and one magazine with courage and vision to look the coronavirus crisis in the eye, and not blink.
And it’s Sweden and Anders Tegnell and Fortune?!
PEOPLE, here’s our situation in a nutshell. We’ve got a pandemic raging, and if we’re going to get through this thing, our species has got to develop herd immunity to COVID-19 — either naturally (as we always have with plagues in the past), or with the aid of a vaccine (which can speed the natural process, and save lives).
This is not optional. It simply must happen, and for the sake of our species’ survival we simply can NOT fail in this task. Everyone is hoping for a vaccine by the end of the year, but every medical person I know is dubious that we will see broad distribution of an effective COVID-19 vaccine without side effects by January 1, 2021 — if ever, for that matter.
So the natural form of herd immunity must loom large in human thoughts on COVID-19. In fact, it may be our only real hope.
But there are a couple features of natural herd immunity that must be noted, starting with the fact that it is free, and requires no multi-billion funding from the government, or anyone else. This is a problem? Well, if you’re heart-broken at the thought that Big Pharma companies like Pfizer and a host predatory stock brokers might not be able to make billions of dollars off this broad global COVID-19 calamity, then you’re not going to be a fan of natural herd immunity.
And here’s another significant detail about the natural herd immunity process. For it to work, many, many people MUST get infected, and then survive and get over it (just as they do following inoculation with the artificial vaccine; the two processes are fundamentally identical here).
Now some people clearly get very sick with COVID-19, as the unfortunate story of Broadway star Nick Cordero illustrates, but we know from Science Daily that between 45 percent and 96 percent of people who test positive for COVID-19 may have asymptomatic coronavirus infections, where they feel fine and many don’t even know they’re “sick”!
Among more than 3,000 prison inmates in four states who tested positive for the coronavirus, the figure was astronomical: 96 percent asymptomatic.
“Up to 95 percent of SARS-CoV-2 infections may be asymptomatic,” which appeared in Scientific Daily on June 12, 2020. The Science Daily story was based on data from the Scripps Research Institute published in Annals of Internal Medicine.
And the CDC Director Dr. Robert Redfield recently acknowledged that his organization underestimated the total number of COVID-19 infections in the spring by more than 90 percent! In other words, it now appears that the total number of people with COVID-19 infections in April was nearly 10 times greater than we thought.
And this further underscores the fact that most — maybe even nearly all — of the people infected with the COVID-19 virus don’t get sick! They just throw the virus off and get on with their lives.
CAN YOU imagine better COVID-19 news?!
This is all very hopeful for fighting coronavirus through natural herd immunity because for natural herd immunity to work, you need many people to get infected, then have them get well with improved immunity.
The fact that the actual number of COVID-19 infected Americans was nearly 10 times as large as previously thought because many of these people were asymptomatics who never felt sick and got over COVID-19 naturally — also suggests that coronavirus may less threatening for broad human populations than originally feared.
For one thing, far bigger COVID-19 infection counts inherently reduce the mortality rate calculated for coronavirus, which was once thought to be significant (although never as significant as the Spanish influenza of 1918). This new view of the dramatically decreased death rate now attributed to coronavirus is expressed by a recent New York Times story, which reported that COVID-19 is now believed to have a mortality rate of a little better than 1/2 of 1 percent, meaning one person in every 200 who catches it may be expected to die from it, statistically speaking.
So how bad is a mortality rate of 1/2 of one percent? Well, basically, among pandemics it compares pretty closely to the Asian flu pandemic of 1957-58, which was another novel coronavirus out of China that swept the globe. The Asian flu killed about 120,000 people in the U.S., but did not shut down the human world.
SO LET me get this straight. We’ve got a kind of a flu-like disease here with a kill rate that our culture already proved it could overcome without lock-downs in 1957? And the vast majority of the people who become infected with this flu-like disease will have asymptomatic infections, and not even know they’re sick while they’re productively building herd immunity?
The responsible public health care path here is unequivocal and clear! We must open the countries up all over the world and let COVID-19 sweep through. We must expect that one half of 1 percent of those infected will die, but that number (the often heart-breaking human cost) is microscopic compared to the kill rate for Bubonic plague of the Middle Ages, which may have killed over 50 percent the population of Europe.
And besides, building broad immunity to COVID-19 in the population IS OUR ONLY PATH THROUGH TO THE OTHER SIDE of this pandemic. We’ve simply got to get to herd immunity, vaccine or no. And the natural herd immunity path — meaning, broad exposure of the population to COVID-19 — is actually the cheapest way our species can buy it — in terms of the human cost, the cultural cost, and the economic cost.
So don’t be afraid, and cower like women and children in the bottom of the boat! You are human beings. You rule this world. Now is the time to show your character and your courage, not your weakness and your hysteria.
AND NOW we have a leading public health official, Anders Tegnell, Sweden’s top virologist, who has said pretty much just this: “send the kids back to school and put away the masks“.
In response to which, I say — hooray for Sweden, Anders Tegnell, Berhard Warner and Fortune for thinking independently!
Don’t see many like them around these parts any more.
 |
August 10, 2020 – Children and the virus: As schools reopen, much remains unknown about the risk to kids and the peril they pose to others, Washington Post
The Washington Post writes that the photos showed up on social media just hours into the first day of school: 80 beaming teens in front of Etowah High School near Atlanta, with not a mask on a single face and hardly six inches of distance between them — let alone the recommended six feet.
Amanda Seghetti, a mom in the area, said her parent Facebook group lit up when the pictures of the seniors were posted. Some people thought the images were cute. Others freaked out. Seghetti was in the latter constituency.
“It’s like they think they are immune and are in denial about everything,” Seghetti said.
Pictures of packed school hallways in Georgia and news of positive tests on the first day of classes in Indiana and Mississippi sparked the latest fraught discussions over the risk the coronavirus presents to children — and what’s lost by keeping them home from school. Friday brought reports of more infections among Georgia students, with dozens forced into quarantine in Cherokee County, among other places.
For months, parents and teachers, epidemiologists and politicians have chimed in with their views on the many still-unanswered questions about the extent to which the virus is a threat to children — and the extent to which they can fuel its spread.
A report from leading pediatric health groups found that more than 97,000 U.S. children tested positive for the coronavirus in the last two weeks of July, more than a quarter of the total number of children diagnosed nationwide since March. As of July 30, there were 338,982 cases reported in children since the dawn of the pandemic, according to data from the American Academy of Pediatrics and the Children’s Hospital Association.
President Trump has repeatedly maintained the virus poses little threat to children.
“The fact is they are virtually immune from this problem,” Trump said Wednesday in an interview with Axios.
Eight months after the World Health Organization received the first report of a “pneumonia of unknown cause” in China, much remains uncertain about the coronavirus and children.
Doctors are more confident that most children exposed to the virus are unlikely to have serious illness, a sentiment backed by a report published Friday by the Centers for Disease Control and Prevention that concluded children are far less likely to be hospitalized with covid-19, the illness caused by the virus, than adults. But when children do fall seriously sick, the burden of illness is borne disproportionately: That same CDC report concluded that Hispanic children are approximately eight times more likely and Black children five times more likely to be hospitalized with covid-19 than their White peers.
Early studies on children and the virus were small and conflicting. But accumulating evidence suggests the coronavirus may affect younger children differently than older ones.
For example,doctors say themultisystem inflammatorysyndrome linked to the virus — known as MIS-C —that has appeared in a small number of children weeks after infectionpresents differently in younger children than in teens and young adults. Infants and preschoolers who have been diagnosed with the syndrome have symptoms mirroring Kawasaki, a disease of unknown cause that inflames blood vessels.In the older group, the consequences appear more severe, with doctors describing it more like a shock syndrome that has led to heart failure and even death.
Several studies suggest adolescence could mark a turning point for how the virus affects youths — and their ability to spread the pathogen.
One paper published in July in the journal JAMA Pediatrics found that children younger than 5 with mild to moderatecases ofcovid-19 had much higher levels of virus in their noses than older children and adults — suggesting they could be more infectious. That study, conducted by doctors at the Ann & Robert H. Lurie Children’s Hospital of Chicago, used data from 145 children tested at drive-through sites in that region.AD
A study out of South Korea examining household transmission also found age-based differences in children. Puzzlingly, it seemed toreach an opposite conclusion about transmission than the Chicago researchers did. Children under age 10 did not appear to pass on the virus readily, while those between 10 and 19 appeared to transmit the virus almost as much as adults did.
Max Lau, an epidemiologist at Emory University tracking superspreader events in the state in collaboration with the Georgia Department of Public Health, said two striking trends have emerged even as work continues on an analysis of recent data.
Disease detectives have found relatively few infections among young children even after the state loosened its coronavirus-related shutdown. Researchers elsewhere have noted there hasn’t been a clear, documented case of a young child triggering an outbreak. In contrast, cases spiked among 15- to 25-year-olds, suggesting they may be driving the spread of the virus.AD
“When the shelter-in-place lifted, they perceived that they could go back to normal life and that’s what I observed,” Lau said.
In May, Jerusalem’s Gymnasia Ha’ivrit high school was the center of a major outbreak that public health officials said seeded transmission to other neighborhoods. In June, an overnight YMCA camp in Georgia was forced to close after 260 of 597 children and staff members tested positive for the virus — an event some experts heralded as a parable for what can happen when young people are allowed to gather without being attentive to wearing masks or maintaining physical distance. At that camp, the first to come down with symptoms and be sent home was a teenage counselor.
Other gatherings among teens have led to smaller outbreaks. In New Jersey, it was a party at a country club that left at least 20 teens infected. In Michigan, health officials said more than 100 teens in three counties have tested positive since mid-July following graduations and other parties.AD
Sadiya S. Khan, an assistant professor of cardiology and preventive medicine at Northwestern University’s Feinberg School of Medicine, said social practices, rather than biology, may explain why teens and young adults appear to be spreading infection.
“They are more likely to be out and about. They are more likely to not have experienced any consequences,” Khan said. “There has been a lot of attention to the fact that people who are older have a worse course and if you’re young, it doesn’t feel as dangerous, so they might think, ‘Why be as careful?’ ”
Khan said she worries schools that don’t enforce mask-wearing and social distancing can be laboratories for superspreader events rippling out to the broader community.
Medical history tells us that children’s role in infectious diseases is not always what we first assume. In 1960, in response to significant deaths among the elderly during the 1957-1958 influenza pandemic, the surgeon general recommended flu vaccines for people 65 and older. It wasn’t until decades later that studies showed that mortality among older people could be reduced by vaccinating the young. In 2002, the CDC recommended flu shots for infants and in 2008 expanded that to school-age children.AD
With the coronavirus pandemic, like any disease outbreak, research takes time, and experts say decisions being made about reopening schools are necessarily being made without the full picture of the risk the virus poses to children.
For example, the CDC’s study of that Georgia YMCA camp did not include detailed tracing of how cases spread among campgoers. Did one teenage counselor spread the virus to the whole camp? Did that counselor infect a few younger children, who in turn infected other younger children?
Similarly, that study did not document what happened to families of the infected when the children returned home. Did they bring the virus back to their families, thereby dispelling the notion that children do not transmit the virus to adults? Or, if infections did spread, was it simply the result of high viral prevalence in Georgia, and not the result of contact with a campgoer?AD
As the case of the Georgia camp illustrates, measuring the risk younger children face in returning to school continues to be an inexact art. Parents are left with the agonizing and anxiety-riddled task of evaluating that potential peril for themselves. And they must weigh the potential health risks of the virus against the educational, social, developmental and economic consequences of children remaining out of the classroom.
Teachers unions from Florida to Ohio have protested plans to fully reopen schools, arguing that even if a few months of data suggests children are not likely to suffer severe outcomes from the virus, they could still pass it to vulnerable adults.
On Aug. 2 — hours before the first day of school — the principal of North Paulding High School near Atlanta sent a letter to parents informing them of coronavirus infections on the football team. Video on the Facebook page for the team’s parent-run booster club showed members of the team, with no masks or distance between them, lifting in a weight room as part of a fundraising event a weekearlier.
On the first day of school, students posted a picture of hallways crammed with unmasked classmates. One student was initially suspended for posting the pictures. The school overturned that suspension Friday.
Within days, the school burst into the national spotlight, and the issue spawned heated arguments in a local Facebook group called “What’s Happening Paulding,” with parents occasionally descending into name-calling and expletive-laced tirades as they argued over whether the pictures should warrant concern. Sunday night, North Paulding High sent a letter to parents announcing the school would be closed to in-person learning for at least two days because of nine cases of the coronavirus.
John Cochran, the father of a ninth-grader and middle-schooler in the Georgia school system, said in an interview he felt it wasn’t safe for his children to attend school in person, in part because multiple adults in their family are immunocompromised.
“That was one thing we stressed to the kids — they’ve got too many adults that they are regularly in contact with who could be in bad shape if they pick this up from them,” Cochran said. “Personally, I didn’t want that on my kids’ conscience that they went to school and got their mother, stepdad, dad or grandparents sick.”
In Georgia’s Cherokee County, where the 80 students gathered for that unmasked photo, Seghetti said she knows she’s in the minority in deciding to keep her 11-year-old son, Kaiden, home from school.
Seghetti said after seeing photos shared by parents from inside schools and learning that two elementary campuses in the district already had reported coronavirus cases — a second-grader Tuesday and a first-grader Wednesday — she is confident she made the right decision.Cherokee County schools spokeswoman Barbara P. Jacoby said the schools have implemented changes to try to keep students safe, including staggering bell times to avoid hall crowding and providing students with two masks each they can wear if they wish.
Karin Jessop’s two children, ages 12 and 13, attended that YMCA day camp at Lake Burton where the residential camp outbreak unfolded. Her children, who were at the camp for four weeks but came home each night, did not get infected; the outbreak was among those who stayed overnight, another reminder of the unpredictability of the spread.
Jessop, a technology company executive, said after news of the outbreak broke, “a lot of moms were getting stressed out about making the wrong decision and worried what people will think.”
“At the end of the day, it’s your family,” she said, adding she believes staying home affects her children’s development, which makes the camp experience worth the risk.
“Many of these kids have been home since March, and if you have super gregarious, extroverted kids, they are used to and need that interaction.”
 |
August 11, 2020 — Why does COVID-19 strike some and not others? Fauci sees an answer in new study, Miami Herald
The Miami Herald reports that Dr. Anthony Fauci, the nation’s leading infectious disease expert,said a new study could explain the extraordinary range that people experience with the novel coronavirus, from having no symptoms at all or a mild case to hospitalization or death.
The discovery, which found potential signs of immunity in people who had previously been exposed to other types of coronavirus, could also expand the hunt for a long-lasting COVID-19 vaccine.
Fauci and other scientists said the study published in Science this month held promising findings for understanding why some individuals exposed to COVID-19 for the first time have a modest reaction to the virus.
The study found that the immune systems of roughly half of its subjects appeared to remember past exposure to other, prevalent coronaviruses, including variants of the common cold, equipping them to respond more quickly to a COVID-19 infection once it appeared.
The findings also offer new insights that could help in developing a vaccine by looking at T cells which help fight the virus.
Currently, all major candidates for a coronavirus vaccine undergoing clinical trials focus on harnessing a single antibody protein that can neutralize the virus.
‘ONE-TWO PUNCH’
Since the coronavirus outbreak began, scientists including Fauci have struggled with the question of why the novel coronavirus hits some people so hard and leaves others unscathed.
“One of the things that I don’t think has been emphasized very much at all during the attempt to address, scientifically, the COVID-19 outbreak, and vaccine development and testing, is that we’ve been focusing very exclusively on the antibody test,” Fauci told McClatchy in a recent interview.“There’s another equally important component of the immune system.”
The study, funded by the National Institute of Allergy and Infectious Diseases which Fauci heads, is one of the first to identify T cell “cross reactivity” in individuals who have previously been exposed to one of the four endemic coronavirus strains, SARS or MERS.
Cells known as “T cells,” which originate in the thymus, serve as a secondary line of defense in the immune system once antibodies have failed or faded away.
“If you look at it metaphorically as an army with different levels of defense, the antibodies prevent the virus from getting in. So that’s kind of like the first line of defense,” Fauci explained. “For those viruses that do escape and infect some cells, the T cells come in and kill the cells that are infected or block them.”
The T cells of individuals who took part in the study recognized the novel coronavirus when it was introduced to their immune systems for the first time.
Angela Rasmussen, a virologist at Columbia University, also explained the immune system in military terms, likening antibodies to infantry and T cells to cavalry.
“None of our soldiers have been trained before this,” Rasmussen said. “But the T cell finding suggests that, maybe the cavalry actually is prepared for this virus. Maybe they already know a little bit about how to fight it. And maybe that’s helping the overall army stave off the invading virus.”
Rasmussen cautioned against overstating the findings of the study, noting that the level of protection among those with T cell memory from other coronaviruses remains unknown. But she nevertheless celebrated the findings.
“It’s a piece of good news, scientifically, because otherwise we’re completely naive to this virus and it’s completely brand new,” Rasmussen said. “If there’s anything that can give us an edge in fighting it, even within our own bodies and immune systems, that to me is great news and is very promising.”
Fauci noted that, while T cells last much longer than antibodies, they do not last forever. Themore recently an individual was infected with another typeof coronavirus, the greater likelihood of someprotection from COVID-19.
Itmay explain the vast differences within older age groups, where scientists have tracked both asymptomatic cases as well as deaths in large numbers.
While one elderly individual might have been exposed to a common coronavirus within the past few years, another may not have had that exposure for decades – and not have the T cell memory that might otherwise provide protection.
“It’s sort of like a one-two punch,” Fauci said. “It’s conceivable that the T cells that you’ve made in response a couple of years ago — three, four, five years ago — when you were exposed to a relatively benign coronavirus that causes the common cold, could actually hang around, and when you’re exposed to the SARS-Coronavirus-2, could have some degree of protection,” he said, referring to the novel coronavirus.
GLOBAL LESSONS
Dr. Shane Crotty, a virologist at the La Jolla Institute for Immunology and senior author on the Science study, said in an interview that the findings could mean that individuals with T cell memory from common colds are having less severe responses to COVID-19 exposure, with their immune systems responding to the new infection more quickly.
“At least part of that immune memory is from people’s immune systems seeing common cold coronaviruses before,” Crotty said. “Most people have had those four common cold coronaviruses some time in their life, and about half of people have immune memory that cross-reacts between those common cold coronaviruses and this new coronavirus.”
The initial findings on T cell memory are already helping global leaders in public health better understand why some regions of the world have been hit harder by the COVID-19 pandemic than others.
Bill Gates, co-founder of Microsoft and of the Bill & Melinda Gates Foundation, told CNN over the weekend that “related coronavirus exposure” has begun to explain the regional discrepancies.
“Within a few months we’ll really understand this,” Gates said. He pointed out that, in Southeast Asia, the prevalence of coronavirus-carrying bats might have increased T cell immunity among the human population. “They probably had this cross protection that meant the spread of the disease was not as strong there,” he said.
But the overall impact of these findings still requires greater research, Crotty said.
“There’s no direct evidence of an effect of these cells on disease severity,” Crotty said, “but we’ve taken the critical steps along the way to test that – showing that these cells exist, and now showing that these cells are not all the same in people, and that, definitely, some of these have memories from exposure to the common cold.”
 |
August 14, 2020 — A mathematical model reveals the influence of population heterogeneity on herd immunity to SARS-CoV-2, Science
Science writes in its Abstract that:
Despite various levels of preventive measures, in 2020, many countries have suffered severely from the coronavirus disease 2019 (COVID-19) pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus. Using a model, we show that population heterogeneity can affect disease-induced immunity considerably because the proportion of infected individuals in groups with the highest contact rates is greater than that in groups with low contact rates. We estimate that if R0 = 2.5 in an age-structured community with mixing rates fitted to social activity, then the disease-induced herd immunity level can be ~43%, which is substantially less than the classical herd immunity level of 60% obtained through homogeneous immunization of the population. Our estimates should be interpreted as an illustration of how population heterogeneity affects herd immunity rather than as an exact value or even a best estimate.
 |
August 15, 2020 – Russia produces first batch of COVID-19 vaccine: Interfax, Reuters
According to Reuters, Russia has produced the first batch of its new vaccine for COVID-19, the Interfax news agency quoted the health ministry as saying on Saturday, hours after the ministry reported the start of manufacturing.
Russia has said the vaccine, the first for the coronavirus to go into production, will be rolled out by the end of this month.
The vaccine has been named “Sputnik V” in homage to the world’s first satellite launched by the Soviet Union. President Vladimir Putin has assured the public that it is safe, adding that one of his daughters had taken it as a volunteer and felt good afterwards.
Moscow’s Gamaleya Institute, which developed the vaccine, said previously that Russia would be producing about 5 million doses a month by December-January, Interfax said.
— Bruce Brown
Editor, Coronavirus Vaccine & Herd Immunity Digest
 |  |  |  |